– Policy Brief
- Both the pandemic threat to physical health and the pandemic control measures constitute stressors that potentially affect mental health.
- There was a sharp increase in the proportion of people with severe depressive symptoms in the pandemic’s second wave in November 2020 compared with the first wave during the lockdown in April 2020.
- Those most affected by mental health problems are young people, those who have suffered financially during the pandemic, and those from the French-speaking part of Switzerland, which was hit hardest by the second pandemic wave.
- Health care workers in intensive care are also at increased risk for mental health problems.
- If the epidemiological situation requires restrictive measures, it is necessary to consider appropriate countermeasures to prevent and counteract potential mental health problems.
Executive summary:
In light of the results of the third survey of the Swiss Corona Stress Study, referring to the period from 11 to 19 November 2020, during which 11,612 people from all over Switzerland participated, we are updating the policy brief on the mental health consequences of the pandemic. Stress levels have increased significantly compared to the first survey during the lockdown in April 2020. The increase in stress was accompanied by an increase in depressive symptoms. Factors associated with psychological stress and depressive symptoms included burdens due to a COVID-19-related change at work, school, or in education, COVID-19-related financial losses, and fears about the future. These stressors have increased significantly compared to the time of the April lockdown. Further factors were the fear that someone in the respondent’s closest circle would become seriously ill or die from COVID-19, as well as the burden of social restrictions and burdens from an increase in conflicts at home. While the proportion of respondents with moderately severe or severe depressive symptoms was 3% before the pandemic, 9% during the April lockdown, and 12% during partial loosening in May, it increased to 18% in November. The risk for moderately severe or severe depressive symptoms was associated with age (with those aged 14-24 showing the highest risk) and was increased in people experiencing financial losses due to COVID-19-related measures. In addition, people from the French-speaking part of Switzerland, which was most affected by the pandemic during the second wave, were at higher risk of moderately severe or severe depressive symptoms than people from the rest of Switzerland. Furthermore, studies from abroad indicate that health care workers in intensive care are at increased risk for mental health problems.
Recommendations to prevent and counteract mental health problems:
- Reduce case numbers and prevent future pandemic waves
- Compensate financial losses due to COVID-19-related measures
- Implement countermeasures to reduce stress in schools/universities
- Maintain coverage of costs for remote psychological/psychiatric treatment
- Continue to increase public awareness for mental health problems and treatment options, and promote evidence-based preventive measures, such as physical activity
Main text
Authors: Dominique de Quervain, Claudine Burton-Jeangros, David Sander, Eva Maria Belser, Pascal Mahon, Suerie Moon, Simone Munsch, Francesco Panese, Philip Rieder, Laura Bernardi, Dario Spini, Samia Hurst
The impact of the pandemic on mental health
The situation in Switzerland
Several studies reported an impact of the lockdown in spring on general wellbeing, social life and stress levels (Moser et al., 2020; Ehrler et al., 2020; Bosshardt et al., 2020; Wissmath, 2020, see Stocker et al., 2020 for review). It is important to note that there was a considerable heterogeneity in reactions to the lockdown. For example, while 50% of participants reported an increase in stress during the lockdown compared to the time before the pandemic, 24% reported no change and 26% even reported a decrease in stress (due to relieving aspects of the lockdown) (de Quervain et al., 2020a). During the partial lifting of the measures in May, fear of coronavirus decreased, but mean stress levels and depressive symptoms remained elevated (de Quervain et al., 2020a).Results of the Swiss Corona Stress Study from November 2020
According to the results of the most recent survey (de Quervain et al., 2020b), stress levels have increased significantly in comparison with the first pandemic wave in spring – the proportion of people experiencing severe stress during the lockdown in April stood at about 11%; in November, this figure was as high as 20%. Depressive symptoms have also increased. The main factors associated with psychological stress and depressive symptoms include changing situations at work, at school or in vocational training due to the pandemic. Further factors include the burden of financial losses, increased conflicts at home, and fears about the future. These factors are reported by respondents to be more burdensome in comparison with the lockdown period in April. Further, study participants found stressful the fear that their loved ones may become seriously ill or even die from COVID-19, and the pressure of social restrictions. The proportion of respondents with moderately severe or severe depressive symptoms (PHQ≥15) was 3% before the pandemic (retrospective rating), 9% during the lockdown and 12% following the easing of restrictions in May, with a rise to 18% in November. Those particularly affected by moderately severe or severe depressive symptoms comprise: – Young people: The prevalence of moderately severe or severe depressive symptoms is 29% in those aged 14-24, 21% in ages 25-34, 17% in ages 35-44, 14% in ages 45-54, 13% in ages 55-64 and 6% in the over 65s (Figure 1).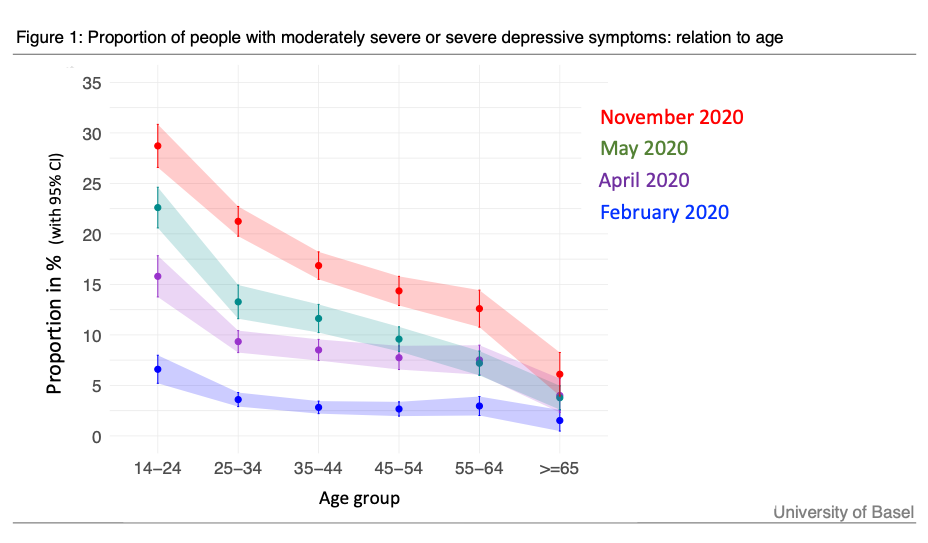
– People working in areas of business affected by the measures imposed by the federal government and the cantons (e.g. restaurants, culture, tourism). With a prevalence of 28%, people who have seen their financial reserves decline are twice as likely to experience severe depressive symptoms as people with unchanged or increased reserves (14%).
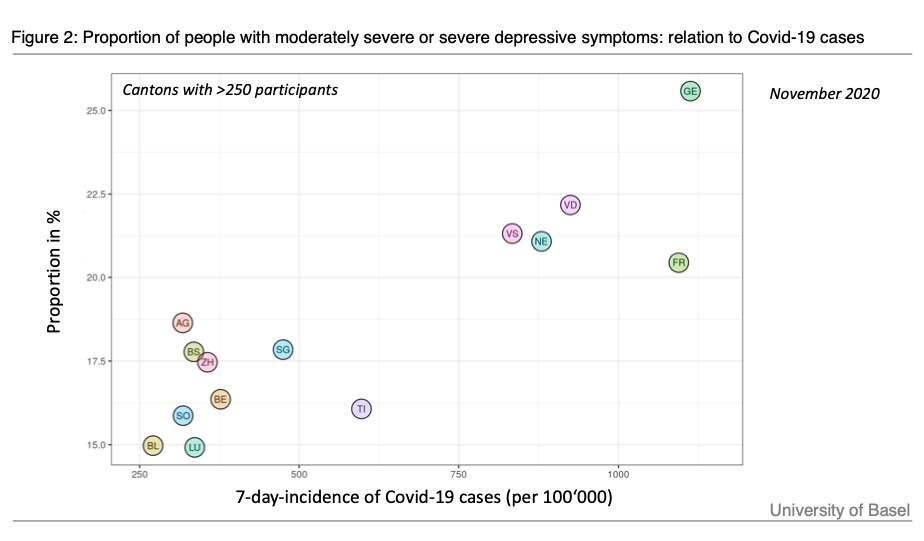
– At 22%, people from French-speaking Switzerland are more strongly affected than those in German-speaking Switzerland, at 17%, or Italian-speaking Switzerland, at 16%. In addition, we found a correlation between the strength of the second wave (incidence of new infections) and the prevalence of depressive symptoms in the cantons (Figure 2). There were no cantonal differences in the prevalence of depressive symptoms during the first wave in April (see de Quervain et al., 2020b, Fig. 5a).
Qualitative feedback from Swiss psychiatric associations
Qualitative feedback from Swiss psychiatric associations (Swiss Conference of Academic Psychiatry, the Swiss Mental Health Care, die Schweizerische Gesellschaft für Kinder- und Jugendpsychiatrie und -psychotherapie, die Schweizerische Vereinigung Psychiatrischer Chefärztinnen und Chefärzte) indicate that there are currently no general bottlenecks in in- or outpatient care in adult psychiatry, but that there is increased demand in child and adolescent psychiatry. In the Department of Child and Adolescent Psychiatry at the Psychiatric University Hospital Zürich, increases in emergency consultations are estimated at 40% compared to 2019 (personal correspondence Prof. Susanne Walitza). From the associations, there is a clear call for maintaining and extending billing options for digital (phone, online) psychiatric and psychological consultations and the establishment of a Swiss-wide monitoring system (personal correspondence Prof. Erich Seifritz). The NCS Task Force supports these positions.Economic perspective
The costs of work-related stress for employers in Switzerland (due to productivity losses) are estimated at CHF 7.6 billion per year (pre-pandemic, Galliker et al., 2020). Added to this are the medical costs due to stress; also those of the non-working stressed part of the population. Considering the doubling in prevalence of people with very high stress levels from April to November 2020 (de Quervain 2020b), the increase in stress during the pandemic results in additional costs estimated at CHF 600 million per month (assuming stress levels as in November 2020). This estimation can be considered conservative as it does not include medical costs and the rise in stress from the time before the pandemic to April 2020.Legal perspective
The Federal Constitution guarantees a right to psychological integrity (Art. 10 para. 2) and obliges all state actors to, first, limit actions having negative impacts on people’s mental health and, second, take necessary measures to protect those suffering from mental health problems. Children and young people enjoy extra rights in this regard. Article 11 of the Federal Constitution obliges federal, cantonal and municipal authorities to offer children and young people “special protection of their integrity and encouragement of their development”. This obligation is in line with the binding obligation of the UN Convention on the Rights of the Child (Art. 24 (1): “States Parties recognize the right of the child to the enjoyment of the highest attainable standard of health and to facilities for the treatment of illness and rehabilitation of health. States Parties shall strive to ensure that no child is deprived of his or her right of access to such health care services.”). While there is no legal human right for all to have access to the health care system they require, constitutional and international law is violated when children below the age of 18 do not have access to the health care their mental situation requires.Public health perspective
From a public health perspective, it is important to consider both physical and mental health. Mental health is affected by both the pandemic-related threat to physical health and the restrictive measures implemented to prevent such a physical threat. Thus, if the epidemiological situation requires restrictive measures, it is necessary to consider appropriate countermeasures to prevent and counteract potential mental health problems.What should be done to monitor, prevent and counteract mental health problems related to the COVID-19 pandemic?
Strategies to reduce the impact of the COVID-19 pandemic and its measures on mental health are needed. They should be targeted towards the whole population in terms of general wellbeing and mental health services and support while providing specific support for vulnerable groups, notably health care workers, those with psychopathological vulnerabilities, young people and those suffering from social isolation (Holmes et al., 2020; Brooks et al., 2020).Recommendations
The NCS Task Force supports the general recommendations listed in the mental health report of the Federal Office of Public Health (Stocker et al., 2020). Furthermore, based on the latest results on the impact of the pandemic on mental health, we have the following specific recommendations:- Reduce case numbers and prevent future pandemic waves
- Compensate financial losses due to COVID-19-related measures
- Implement countermeasures to reduce stress in schools/universities
- Maintain coverage of costs for remote psychological/psychiatric treatment
- Continue to increase public awareness for mental health problems and treatment options, and promote evidence-based preventive measures, such as physical activity
References
Anderson et al., (2014) Stress in America. Are Teens Adopting Adults’ Stress Habits? American Psychological Association https://www.apa.org/news/press/releases/stress/2013/stress-report.pdf
Bosshardt, L., Bühler, G., Craviolini, J., & Hermann, M. (2020). Altas der Emotionen, im Auftrag der «Wie geht’s dir?»-Kampagne. Forschungsstelle sotomo.
Brooks, Samantha K, Rebecca K Webster, Louise E Smith, Lisa Woodland, Simon Wessely, Neil Greenberg, and Gideon James Rubin. 2020. “The Psychological Impact of Quarantine and How to Reduce It: Rapid Review of the Evidence.” The Lancet 395 (10227): 912–20. https://doi.org/10.1016/S0140-6736(20)30460-8.
Choi et al., 2020. Assessment of Bidirectional Relationships Between Physical Activity and Depression Among Adults A 2-Sample Mendelian Randomization Study. JAMA Psychiatry. 2019;76(4):399-408. doi:10.1001/jamapsychiatry.2018.4175
Ehrler, Monsch, Steinmetz (2020). FORS Covid-19 Erhebungen, Faktenblatt No1. Wohlbefinden und Sorgen während dem Lockdown. FORS. https://forscenter.ch/wp-content/uploads/2020/09/factsheet_wellbeing.pdf
Galliker et al., Job-Stress-Index 2020, https://gesundheitsfoerderung.ch/assets/public/documents/de/5-grundlagen/publikationen/bgm/faktenblaetter/Faktenblatt_048_GFCH_2020-09_-_Job-Stress-Index_2020.pdf
Gunnell, David, Louis Appleby, Ella Arensman, Keith Hawton, Ann John, Nav Kapur, Murad Khan, Rory C O’Connor, Jane Pirkis, and COVID-19 Suicide Prevention Research Collaboration. 2020. “Suicide Risk and Prevention during the COVID-19 Pandemic.” The Lancet. Psychiatry 7 (6): 468–71. https://doi.org/10.1016/S2215-0366(20)30171-1.
Holman, Thompson, Garfin, Silver, The unfolding COVID-19 pandemic: A probability-based, nationally representative study of mental health in the United States
Science Advances 2020 Oct 14;6(42):eabd5390. doi: 10.1126/sciadv.abd5390. Print 2020 Oct.
Holmes, Emily A, Rory C O’Connor, V Hugh Perry, Irene Tracey, Simon Wessely, Louise Arseneault, Clive Ballard, et al. 2020. “Multidisciplinary Research Priorities for the COVID-19 Pandemic: A Call for Action for Mental Health Science.” The Lancet Psychiatry 7 (6): 547–60. https://doi.org/10.1016/S2215-0366(20)30168-1.
Hurst et al., Psychological effects of confinement and deconfinement. Policy Brief, Swiss National Covid-19 Science Task Force, 14.06.2020
Inchley et al., Spotlight on adolescent health and well-being. Findings from the 2017/2018 Health Behaviour in School-aged Children (HBSC) survey in Europe and Canada. International report. Volume 2. Key data. Copenhagen: WHO Regional Office for Europe; 2020. Licence: CC BY-NC-SA 3.0 IGO.
Knittel, Schneidenbach, Mohr, Zuviel Stress – zuviel Druck! Wie Schweizer Jugendliche mit Stress und Leistungsdruck umgehen. JUVENIR-STUDIE 4.0 EINE STUDIE DER JACOBS FOUNDATION https://jacobsfoundation.org/app/uploads/2017/07/Juvenir-4.0_Langfassung_DE_final.pdf
Mengin, A, M C Allé, J Rolling, F Ligier, C Schroder, L Lalanne, F Berna, et al. 2020. “Psychopathological consequences of confinement.” L’Encephale 46 (3S): S43–52. https://doi.org/10.1016/j.encep.2020.04.007.
Moser, A. (2020, Oktober 11). Zeitnahes Monitoring der Auswirkungen der Covid-19-Krise auf die Gesundheit und das Leben der Bevölkerung in der Schweiz. Covid-19 Social Monitor. https://csm.netlify.app/post/trend/
Palsson, Ballou, Grey. “The U.S. National Pandemic Emotional Impact Report Findings of a nationwide survey assessing the effects of the COVID-19 pandemic on the emotional wellbeing of the U.S. adult population.” June 2020.
Pierce, Hope, Ford, Hatch, Hotopf, John, Kontopantelis, Webb, Wessely,
McManus, M Abel, “Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population”. Lancet Psychiatry 2020; 7: 883–92.
de Quervain et al., 2020a. “The Swiss Corona Stress Study.” Preprint. Open Science Framework. https://doi.org/10.31219/osf.io/jqw6a.
de Quervain, et al. 2020b. “The Swiss Corona Stress Study: second pandemic wave, November 2020” Preprint. Open Science Framework. https://osf.io/6cseh/.
Saracoglu, Simsek, Kahraman, Bombaci, Sezen, Saracoglu, Demirhan. 2020.
The Psychological Impact of COVID-19 Disease is more Severe on Intensive Care Unit Healthcare Providers: A Cross-sectional Study. Clin Psychopharmacol Neurosci. 2020 Nov 30;18(4):607-615. doi: 10.9758/cpn.2020.18.4.607.
Simon and Eicher 2020. Protecting physical and mental health of healthcare workers. Policy Brief, Swiss National Covid-19 Science Task Force, 14.06.2020
Stocker, D., Jäggi, J., Liechti, L., Schläpfer, D., Németh, P., & Künzi, K. (2020). Der Einfluss der COVID-19-Pandemie auf die psychische Gesundheit der Schweizer Bevölkerung und die psychiatrisch-psychotherapeutische Versorgung in der Schweiz. Erster Teilbericht. Bern: Bundesamt für Gesundheit.
Taquet, Luciano, Geddes , Harrison 2020. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. 2020 Nov 9;S2215-0366(20)30462-4. doi: 10.1016/S2215-0366(20)30462-4.
Vahia, Jeste, Reynolds. 2020. Older Adults and the Mental Health Effects of COVID-19. JAMA; 324(22):2253-2254. doi: 10.1001/jama.2020.21753.
Wissmath, Mast, Kraus, Weibel. 2020.” Understanding the psychological impact of the COVID-19 pandemic and containment measures: an empirical model of stress”. medRxiv. https://doi.org/10.1101/2020.05.13.20100313
Date of request: –
Date of response: –
Experts involved: Public Health; Ethics, legal, social
Contact persons: Dominique de Quervain, dominique.dequervain@unibas.ch