– An updated version will be published in February 2021.
Executive summary
This document builds on the policy brief (PB) and recommendations of the Swiss National Covid-19 Science Task Force (NCS-TF) of 12 August 20201 on the role of children and adolescents (0-18 years of age) in the transmission of SARS-CoV-2. The focus is on the SARS-CoV-2 testing strategy for children (0-12 years of age) and the quarantining strategy for children and adolescents in Switzerland. The present recommendations take into account all respective evidence and the epidemiological situation as of 10 December 2020 and are largely based on the previous NCS-TF evaluation of the scientific evidence about the pediatric infectiousness of and susceptibility to infection with SARS-CoV-2. The NCS-TF has always stressed and maintained the fundamental right to education and the societal benefits of education (see previous PBs as well as the Task Force’s recommendations from 23 October 20201,2). This document supports the aim to keep compulsory schools open wherever possible, and for upper secondary and tertiary level students to be preferably taught online during times of high transmission in specific areas.
1. Short summary of the available evidence based on the Swiss National COVID-19 Science Task Force’s policy brief from 12 August 20201</sup
- Children and adolescents can become infected by SARS-CoV-2 but usually develop milder symptoms than adults. A majority of SARS-CoV-2 positive children is however symptomatic.
- There is still limited evidence as to what extent children transmit SARS-CoV-2. However, all the available evidence shows that children (<12 years) are not the main drivers of this pandemic. Consequently, there is probably only a little effect of school closures on the course of this pandemic. Pandemic school closures for children had little effect on slowing the pandemic.
- Studies from the 2020 SARS-CoV-2 spring wave suggest that children are possibly less prone to becoming infected by SARS-CoV-2 than adults.3
- Adolescents and young adults (>12 years) appear more susceptible to infection than children, have higher viral loads, show greater mobility and have many close contacts. Hence in conjunction with the fact that they usually develop mild symptoms of SARS-CoV-2 they could play an important role in transmission.
[1] The role of children and adolescents (0-18 years of age) in the transmission of SARS-CoV-2 (12 August 20 -EN): https://ncs-tf.ch/de/policy-briefs?layout=default
[2] Beurteilung der Lage, 23. Oktober 2020: https://ncs-tf.ch/de/policy-briefs?layout=default
[3] Comprehensive community-based studies measuring viral loads or exposure show comparable prevalence between children and adults (e.g. Wagner et al. (2020)). These studies do, however, not provide further evidence on children’s proneness to infection as they do not analyze the household settings where the risk for children to become infected is highest.
2. Summary of the current testing and quarantining strategy for schools and day care facilities in Switzerland
The current testing and quarantining strategy is meant to rapidly identify children and adolescents with SARS-CoV-2 or contacts of confirmed SARS-CoV-2 cases and to reduce their possible transmission potential.
Testing:
Figure 1 shows the testing strategy for children <12 years of age (created by the Federal Office of Public Health (FOPH) together with the pediatric specialists; German version attached). The testing strategy for children <12 years of age defines:
a) which children should not attend school/day care;
b) which children should see a pediatrician;
c) which children should be tested for SARS-CoV-2 as determined by the pediatrician in conjunction with the parents.
It needs to be mentioned that by officially recommending to only test children with more severe symptoms (e.g. newly developed fever and other potential COVID-19 symptoms) or symptoms (e.g. cough) lasting ≥3 days, the risk for in-school transmission is likely kept low, as based on current data asymptomatic or mildly symptomatic adults and children have lower viral loads (Liu et al. (2020); Han et al. (2020); Zheng et al. (2020)). There is, however, still no conclusive evidence on the association between viral load and transmission risk in children.
Quarantine:
Children and adolescents have to quarantine for 10 days if they were in close contact with a confirmed SARS-CoV-2 case (<1.5 meters for >15 minutes). As the risk for child-to-child transmission in school and day care settings is relatively low and therefore probably without major societal consequences (see policy brief from 12 August 2020, link on page 1; SAGE (2020)) and as non-invasive public health measures such as physical distancing or mask wearing are difficult to implement without impairing primary school children’s proper social development, these non-invasive public health measures are currently not suggested for children attending compulsory schools in Switzerland. Due to the higher risk of teachers transmitting the virus compared to students, teachers are recommended to keep a 1.5 m distance from their students and adult colleagues and to always wear masks.
Currently, when a student becomes sick and is confirmed to be SARS-CoV-2 positive, it is up to the cantonal physicians to decide whether there is a possible sign of SARS-CoV-2 transmission in the class or school. If ≥2 children or adolescents or the teacher become sick or were potentially sick with SARS-CoV-2 up to two weeks before the index case became sick and if there is no indication that cases originated from outside the school and transmission at the school is assumed, the cantonal physician may order the whole class to be quarantined.
This approach represents a risk-benefit balance between the lower risk of transmission by SARS-CoV-2 positive children and adolescents (0-15 years of age) and the resulting limited risk of cluster developments in compulsory education on the one hand and the importance of finding the majority of cases and tracing transmission routes on the other hand while still granting equal access to education.
3. Critical assessment of the current strategies
- a Testing
- Despite the national guidelines expressively stating that schools and day care centers are not allowed to require a test, many educational facilities currently define their own requirements as to when a negative test is required for children to return to school or day care.
This puts pressure on parents who are to a large extent subject to the economic consequences of having to stay at home (not all jobs are compatible with working from home) to take care of their children when these present with symptoms of an upper respiratory tract infection. These parents will consequently want their children to be tested immediately.
The cold season is expected to cause an increase of children presenting with flu-like symptoms, which might strain Switzerland’s testing resources (particularly personnel performing the tests). - The symptoms of pediatric upper respiratory tract infections that are not caused by SARS-CoV-2 usually persist for more than 3 days. Currently, upon initial presentation with such symptoms a child is required to stay at home for 3 days to see whether the symptoms improve. If the symptoms improve and the child is afebril for >24 hours, then it can go back to school. If the symptoms do not improve, testing is required.As upper respiratory non-SARS-CoV-2 symptoms usually persist for more than 3 days (as mentioned above) the majority of these children would be tested after 3 days according to the current guidelines. This leads to (i) children being kept out of school for 3 days, depriving them of their right to education, and (ii) an economic strain on the family’s finances or the job situation of the parent who needs to stay home and care for the child.
While it might be ideal to thus test every child presenting with the symptoms of an upper respiratory tract infection, this will not be feasible due to limited testing resources (particularly personnel performing the tests). It needs to be highlighted that the mass testing of mildly symptomatic children (<12 years of age) will probably not affect the course of the pandemic (as also seen in other countries like the Netherlands that are e.g. no longer testing these children and are not reporting major school outbreaks4). It will, however, disproportionally strain Switzerland’s testing resources (particularly personnel as well as consumables) on a population that based on current data is not the main driver of this pandemic.5
b. Quarantine
The current quarantining strategy risks leading to numerous children being quarantined when cases in the general population and consequently inevitably in the pediatric population rise. The number of ≥2 children being positive in one class is very low and there is no certainty of them having been infected in the classroom (SAGE (2020)). As parents and other close contacts of SARS-CoV-2 positive children are not regularly tested as a means of finding the transmission chain, this way of transmission is hardly taken into account. According to all available data children are, however, mostly infected within their families and not in schools (also see the policy brief from 12 August 2020). 6 / 7
Quarantine in Switzerland is meant to be spent indoors in the respective homes with children only being allowed outside for short periods 8. Children from lower income families with small apartments are most vulnerable and will be affected by this lack of space. This will in turn affect their physical and mental wellbeing (e.g. increase in anxiety) and thus their development with repeated lack of movement potentially also leading to stress and other mental health problems (Imran et al. (2020); SAGE (2020)). Frequent quarantine will have a negative effect on children’s development and as a consequence on Swiss society in the future.
As already observed during the 2020 spring lockdown when schools were closed repeated quarantine impacts children’s chance at an equal education as distance teaching requires the correct equipment and knowhow (internet access, computer/laptop, computer skills), a quiet place to study and parents who can provide educational support since teachers are less readily available (European Commission (2020); Andrew et al. (2020); SAGE (2020)).
Repeated quarantine will thus not only have a major negative effect on children but will also affect the whole family and its social and economic life. Smaller children cannot stay at home alone, which means that one parent has to take care of them. As already seen during the spring lockdown this can put a sudden high strain on working parents, as manyrofessions require physical attendance and are not compatible with working from home. Even if working from home is possible, taking care of a child and working at the same time will not only lead to less productive work but it will more importantly also lead to more stress (both economic and emotional) for the respective parent and the whole family (CDC (2020)).
[4] This recommendation is based on data from the Dutch health authorities showing that children (<15 years of age) are not driving the pandemic and while they can spread SARS-CoV-2 their risk is much lower than the risk of people >15 years of age (RIVM (2020)).
[5] Data from the Swedish health authorities sees around 1-2% of mildly symptomatic children testing positive for SARS-CoV-2 even during times of higher community transmission. Exemplary data from the University Children’s Hospital Basel (UKBB) shows an even lower number (<1%) of children with mild symptoms of an upper respiratory tract infection testing positive for SARS-CoV-2 during months of low/moderate community transmission in Switzerland (Re 0.85-1.9) (June-September 2020) (https://ncs-tf.ch/de/lagebericht).
[6] Children from weaker socioeconomic backgrounds probably have a higher exposure risk to SARS-CoV-2 at home than children from less disadvantaged families. Possible reasons include that their parents work in lower-income jobs that cannot be done remotely, which increases the parents’ own risk of SARS-CoV-2, and that they live in smaller living quarters, where social distancing is not possible (Patel et al. (2020)). This can explain the higher rates of SARS-CoV-2 positive children from weaker socioeconomic backgrounds (Wagner et al. (2020)).
[7] Data from the UK describing an increase in cases in school-aged children shows that the pediatric cases followed a potential increase in overall community transmission before schools were reopened further hinting at children being infected within their families and not in schools (SAGE (2020)).
[8] BAG-recommendation (only available in German): “COVID-19: Anweisungen zur Quarantäne“ (https://www.bag.admin.ch/bag/de/home/krankheiten/ausbrueche-epidemien-pandemien/aktuelle-ausbrueche-epidemien/novel-cov/isolation-und-quarantaene.html)
4. Recommendations
- Compulsory schools are to be kept open. A potential closure must be seen as an absolute last resort for areas/schools/classes with high case numbers. Should it, at some point during the pandemic, become necessary to consider closing compulsory schools (due to a high number of SARS-CoV-2 positive children and/or teachers in specific areas) the following principles need to apply:
- Schools or classes with high case number in teachers and/or children should start distance learning whenever possible. They should only return to school if the epidemiologic situation of the specific area/school/class allows it.
- For children whose families do not have the resources for effective and successful online teaching (e.g. no laptop, no internet, no place to study or who may be facing other difficulties in acquiring an education at home appropriate compensatory measures should be taken such as still being taught at schools.
- Recommendations on when children should stay at home, when they should be tested and when they have to quarantine should be consistently made at the national level. They should then be implemented exclusively by medical professionals and cantonal physicians and cannot be left to schools and/or parents.
- Sick children are to stay at home and not go to school as long as they display acute symptoms (decision of when to return to school: see previous point).
- Quarantine should be reserved for the children who are close contacts of a single confirmed case (day care and school settings included).
- Resulting from the low risk of student-to-student as well as student-to-teacher transmission, the definition of close contacts in compulsory school settings must be adapted (e.g. closest companions/group of companions/companions children spend more time with, babysitters, students sitting next to each other). In case of a SARS-CoV-2 positive student these close contacts must be tested and quarantined while the rest of the class should only be tested but not quarantined (right to education).
- To alleviate the economic impact of parents being unable to go to work when they have to care for their sick or quarantined children, federal compensation to companies/parents should be established and implemented.
- Schools and teachers should be aware that the current situation, including social restrictions, wearing masks and sick leave, puts additional psychological pressure on children impacting their receptiveness to teaching. The schools should address these aspects in appropriate ways particularly by handling the curriculum more flexibly.
- Most scientific evidence differentiates between larger age groups (e.g. studies comparing 0-9 year olds vs. 10-19 year olds). To better tailor decision-making to the Swiss school system Swiss-wide studies should be performed analyzing narrower age groups (e.g. 0-5 years olds vs. 6-12 year olds etc.).
- The best approach to break transmission chains is to encourage and implement broad and comprehensive testing, particularly when more feasible new types of tests (e.g. buccal swabs or saliva-based tests) become fully validated and are broadly available for this age group. They will make testing more children in a shorter time period more feasible and will thus facilitate swift strategic decision making in school and day care settings. However, if the testing capacity proves to be insufficient (e.g. when there is not enough personnel to perform the tests), testing should prioritize the following pediatric groups:
- Children who are severely sick (e.g. fever and shortness of breath or fever and severe cough)
- Children who were close contacts of confirmed SARS-CoV-2 cases
- Children whom the cantonal physicians want to be tested as part of an outbreak investigation
- Children who are admitted to hospitals
- Teachers and staff need to wear a mask and keep a 1.5 meter distance from students and staff.
- Children from lower secondary education onwards, generally ≥12 years, need to wear a mask and keep 1,5 meters distance; an arms-length distance9 to classmates and staff.
- In accordance with the World Health Organization’s recommendations children attending primary education
- Should aim for an arms-length distance in classrooms to classmates and staff and
- Can wear masks for a limited time (e.g. specific school lessons)
- Distance learning for students from upper secondary and tertiary education is recommended in times of high community transmission. If face-to-face learning is provided for children/adolescents facing difficulties with distance learning it should take place in very well-ventilated rooms and both students and teachers should keep a 1.5 meter distance from each other and wear masks whenever they are in the educational facility.
- Parents should minimize time spent on school premises, wear masks and strictly adhere to hygiene and social distancing rules.
- Teachers and staff should minimize the time interacting with colleagues and should otherwise also strictly adhere to hygiene and social distancing rules.
- The use of the SwissCovid App should be highly recommended in higher education settings.
- Compulsory equipping of schools with hand washing and hand disinfection stations
- No hand shaking with teachers
- More frequent rigorous cleaning of the school; particularly toilets and changing rooms
- Thoroughly and regularly ventilate closed rooms such as classrooms and halls (at a minimum before starting school in the morning and in every break)
- Prevent in principle the spontaneous mixing among classes during recess, for example by staggering the time of recess by grade or defining separate recess areas (the mixing of groups to form another class, e.g. for MINT (mathematics, information technology, natural sciences, technology) or sports classes results in another known group and does consequently not need to be avoided)
- Avoid high-contact activities, activities with close proximity to other students and activities associated with high viral emissions in upper secondary and tertiary education (e.g. team sports with tackling such as basketball and football, choirs, etc.)
- Whenever possible have sport lessons outside
- Ventilate changing rooms regularly, consider changing in other rooms or at home to avoid crowding
- Stagger lunch hours or allow children to go home for lunch (day schools included) [9] Estimating the distance of 1.5 meters might prove challenging for children, so the more feasible approach to keep an „arms-length distance“ was adopted.
References
Andrew, Alison, Sarah Cattan, Monica Costa Dias, Christine Farquharson, Lucy Kraftman, Sonya Krutikova, Angus Phimister, and Almudena Sevilla. “Inequalities in Children’s Experiences of Home Learning during the COVID-19 Lockdown in England,” August 17, 2020. https://www.ifs.org.uk/uploads/publications/wps/WP202026-Inequalities-childrens-experiences-home-learning-during-COVID-19-lockdown-England.pdf. |
CDC. “Ensure Children’s Wellbeing During COVID-19: Parental Resources |CDC.” Centers for Disease Control and Prevention. Centers for Disease Control and Prevention, September 16, 2020. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/parental-resource-kit/index.html. |
European Commission. “Educational Inequalities in Europe and Physical School during Covid-19 .” Accessed November 9, 2020. https://ec.europa.eu/jrc/sites/jrcsh/files/fairness_pb2020_wave04_covid_education_jrc_i1_19jun2020.pdf. |
Han, Mi Seon, Moon-Woo Seong, Namhee Kim, Sue Shin, Sung Im Cho, Hyunwoong Park, Taek Soo Kim, Sung Sup Park, and Eun Hwa Choi. “Viral RNA Load in Mildly Symptomatic and Asymptomatic Children with COVID-19, Seoul.” Emerging Infectious Diseases 26, no. 10 (June 4, 2020). https://doi.org/10.3201/eid2610.202449. |
Imran, Nazish, Irum Aamer, Muhammad Imran Sharif, Zubair Hassan Bodla, and Sadiq Naveed. “Psychological Burden of Quarantine in Children and Adolescents: A Rapid Systematic Review and Proposed Solutions.” Pakistan Journal of Medical Sciences 36, no. 5 (2020). https://doi.org/10.12669/pjms.36.5.3088. |
Liu, Yang, Li-Meng Yan, Lagen Wan, Tian-Xin Xiang, Aiping Le, Jia-Ming Liu, Malik Peiris, Leo L M Poon, and Wei Zhang. “Viral Dynamics in Mild and Severe Cases of COVID-19.” The Lancet Infectious Diseases 20, no. 6 (March 19, 2020b): 656–57. https://doi.org/10.1016/s1473-3099(20)30232-2. |
Patel, J.a., F.b.h. Nielsen, A.a. Badiani, S. Assi, V.a. Unadkat, B. Patel, R. Ravindrane, and H. Wardle. “Poverty, Inequality and COVID-19: the Forgotten Vulnerable.” Public Health 183 (2020): 110–11. https://doi.org/10.1016/j.puhe.2020.05.006. |
National Institute for Public Health and the Environment. “Children, School and COVID-19.” RIVM – Committed to health and sustainability, November 2, 2020. https://www.rivm.nl/en/novel-coronavirus-covid-19/children-and-covid-19. |
Scientific Advisory Group for Emergencies (SAGE). “Children’s Task and Finish Group: Update on Children, Schools and Transmission,” November 13, 2020. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/935125/tfc-covid-19-children-transmission-s0860-041120.pdf. |
Wagner, Michael, Robert Krause, Peter Willeit, and Bernd Lamprecht. “Ergebnisse Der Erstuntersuchung Der Schul-SARS-CoV-2-Monitoringstudie,” 2020. https://start.univie.ac.at/fileadmin/user_upload/startseite/Dokumente/Coronavirus/Schul-SARS-CoV-2-Studie-Analyse_Abstract_PA.pdf. |
World Health Organization. “Coronavirus Disease (COVID-19): Children and Masks,” August 21, 2020. https://www.who.int/news-room/q-a-detail/q-a-children-and-masks-related-to-covid-19. |
Zheng, Shufa, Jian Fan, Fei Yu, Baihuan Feng, Bin Lou, Qianda Zou, Guoliang Xie, et al. “Viral Load Dynamics and Disease Severity in Patients Infected with SARS-CoV-2 in Zhejiang Province, China, January-March 2020: Retrospective Cohort Study.” Bmj, April 21, 2020, m1443. https://doi.org/10.1136/bmj.m1443. |
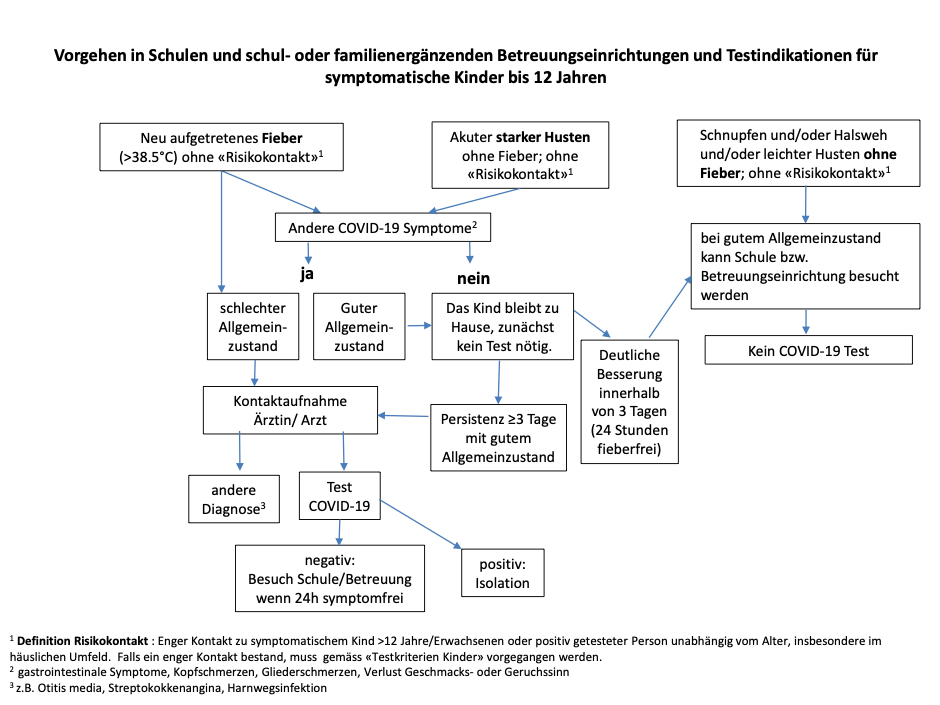
Figure 1 Flowchart of when to test children with the symptoms of an upper respiratory tract infection (published by the Federal Office of Public Health (FOPH) together with the pediatric specialists)
Date of request: 23/10/2020
Date of response: 10/12/2020
In response to request from: NCS-TF Advisory Board
Expert groups and individuals involved: All with Public Health in lead
Contact persons: Margarethe Wiedenmann, Marcel Tanner, Roman Stocker