26 September 2020 – Policy Brief
Summary of request/problem
It is probable that SARS-CoV-2 will be circulating during the influenza season 2020/21. This situation might result in a double burden of disease with both viruses spreading, causing similar symptoms. It is, therefore, crucial that we have plans in place to protect those at risk, prevent ill health, and minimize the impact on the health care system. A question submitted by the cantonal health authorities /GDK to the NCS-TF relates to this issue: “What is the importance of influenza vaccination concerning COVID-19?”.
Executive summary
- Both influenza and COVID-19 are respiratory viral infections. They share symptoms (e.g., fever, cough) and approaches to prevention (e.g., hand hygiene,staying home when sick, physical distancing, respiratory etiquette). Further, risk groups for influenza and COVID-19 are similar;both include olderpeople and people with chronic illnesses.
- Influenza vaccination has been shown to prevent death, morbidity, hospital admissions,particularly among chronically ill people, but also in children and pregnant women. The Federal Office of Public Health (FOPH) has had influenza vaccine recommendations in place for several years. These target older adults, but also those with chronic illnesses, premature infants, pregnant women, residents in long-term health care facilities or those in regular contact with vulnerable populations, most importantly,healthcare workers.
- Already in 2003,the World Health Assembly adopted a resolution urging member states to “increase influenza vaccination coverage of all people at high risk and to attain coverage of 75% among the elderly by2010.”Unfortunately,in Switzerland, influenza vaccination coverage is low in older and chronically ill people, and also low in healthcare workers(around 30-40%).
- We recommend implementing strategies to substantially increase the vaccination coverage for influenza for the upcoming influenza season. Strategies should target the risk groups for both influenza and COVID-19, their contacts, as well as health care workers. Because shortages of influenza vaccination are likely in the coming season, clear vaccination priorities should be defined. The strategies should be promoted on a national level using effective communication. In parallel, strategies that include the vaccination of children should be evaluated.
Introduction
Seasonal influenza
Seasonal influenza isa challenge for surveillance, control,and treatment[1,2]. Worldwide, it causes 3 to 5 million cases of severe illness each year and kills from 250,000 to 500,000 people[3], particularly infants, the elderly, and the chronically ill. In Switzerland, influenza is responsible for 111,000 to 331,000 medical consultations yearly and 1,000to 5,000 hospitalizations[4].
Influenza and COVID-19
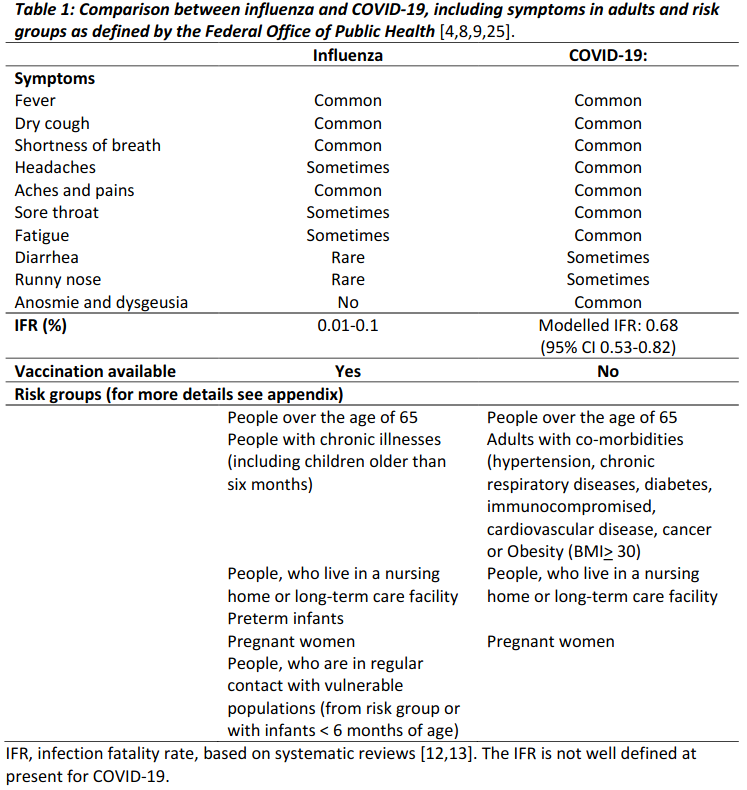
Both influenza and COVID-19 are contagious respiratory diseases caused by viruses,and they share some of the same symptoms (e.g., fever, cough) and approaches to prevention (e.g., hand hygiene, staying home when sick, physical distancing, respiratory etiquette)[5,6]. Further,risk groups for influenza and COVID-19 are similar and include older adults and people with chronic illnesses (Table 1)[4,7–9]. There are also important differences:super spreader events are more common for COVID-19[10,11]; the infection fatality rate is higher for COVID-19[12,13],and transmission during the pre-symptomatic phase is considered more important for COVID-19than for influenza[2,14].
Data on COVID-19 in children and adolescents remain scarce. Studies in children and adolescents showed that COVID-19 disease was generally mild [15–17]. Only very few children develop severe disease requiring ICU admission and ventilation [18]. The available evidence indicates that younger children are less likely to transmit SARS-CoV-2 comparedto adolescents and adults [17]. This is in contrast to seasonal influenza where transmission rates in children and adolescents are high, for example in schools, and children and adolescents frequently transmit the virus to parents and grandparents [19–22].
In the UK, the national vaccination programme for influenza based on an intranasal live attenuated influenza vaccine (LAIV) was extended to include healthy children and adolescents aged 2 to <17 years [23]. The programme’s positive impact on influenza-related outcomes has been documented, both in terms of providing direct protection to children and indirect protection to the wider population, including risk groups. Interestingly, beneficial effects were also evident in the 2014/15 influenza season, despite the circulation of drifted A and B influenza strains [24]. In the USA, several school-based influenza vaccination studies showed relative reductions in influenza-like illness in both children and adults, school days lost and in adult workdays lost [21].
COVID-19 will be circulating during the upcoming influenza season 2020/21. This situation might result in a double burden of disease with both viruses spreading, causing similar symptoms. It is, therefore important that we have effective plans in place for the 2020/21 influenza season to protect those at risk, prevent ill health, and minimize the further impact onthe health care system.
Influenza vaccination
Influenza vaccination and recommendation by the FOPH
Influenza vaccination has been shown to prevent death, morbidity, hospital admissions,and other negative health-related outcomes, particularly among chronically ill people[26–31], but also in children[32]and pregnant women[33].
The Federal Office of Public Health (FOPH) has had influenza vaccine recommendations in place for many years. The recommended indications target mainly older adults, but also patients of any age with chronic illnesses (including children older than six months), premature infants, pregnant women, and residents in long-term health care facilities or those who are in regular contact with the mentioned vulnerable populations, including health care workers[4,9]. Importantly,in 2003, the World Health Assembly adopted a resolution urging member states to”increase influenza vaccination coverage of all people at high risk and to attain coverage of 75% among the elderly by 2010″[7].
Trends of influenza vaccinations status over time in Switzerland
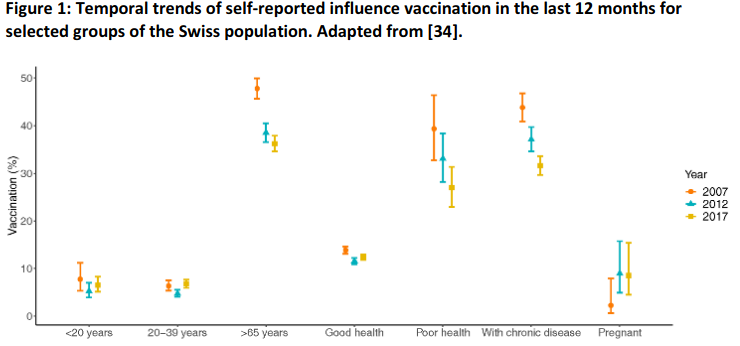
A recent preprint reports trends and associations of sociodemographic characteristics and health-related factors with influenza vaccination practices in Switzerland, based on data from the Swiss Health Surveys2007, 2012,and 2017[34]. The proportion of survey participants reporting a history of influenza vaccination overall was 31.9% (95% confidence intervals 31.4-32.4%). It dropped from 34.5% in 2007 to 28.8% in 2017. The overall uptake of vaccination for influenza within the past 12 months was 16% in 2007 and around 14% in 2012 and 2017. In people with chronic disease, uptake dropped from 43.8% in 2007 to 37.1% in 2012 and 31.6% in 2017 (p<0.001). In older people (≥65 years), uptake dropped from 47.8% in 2007 to 38.5% in 2012 to 36.2% in 2017 (p<0.001). A decrease over time was also seen in those with poor health status (Figure 1).
COVID-19 and seasonal influenza: implications for prevention
The majority of the population remains susceptible to SARS-CoV-2, even in regions with a high burden of COVID-19 cases. For example, sero-surveys from Geneva showed a SARS-CoV-2 seroprevalence of 10·8% (95% CI 8·2–13·9) for their 5thstudy week in May 2020[35]. The stress on health care systems will be greatest should the COVID-19 and influenza epidemic overlap and peak around the same time.
A modelling study from China examined the impact of mass influenza vaccination on COVID-19 epidemics with limited detection capabilities [36]. The modelling examined the effect of mass influenza vaccination on the spread of COVID-19 should an outbreak coincide with the influenza season. The authors found that increasing influenza vaccine uptake or enhancing the non-pharmaceutical public health interventions would facilitate the management of respiratory outbreaks coinciding with the peak flu season. In particular, such an increase in vaccine uptake could partly compensate for the shortage of diagnostic resources.
In Australia,the COVID-19 related increase in non-pharmaceutical interventions (NPIs) such as improved hand hygiene and social distancing appears to have had a substantial impact on the mortality of seasonal influenza [37]. From January to June 2020, there were just 36 deaths from the flu, compared to 430 deaths in the same period in 2019. School closures and border closures probably also played a role in reducing influenza transmission.Similarly, in Singapore, influenza activity declined steeply following the implementation of NPIs [38]. The experience in Australia and Singapore shows that NPIs are effective measures to reduce transmission of both influenza and COVID-19.
Conclusion and Recommendations
The stress on health care systems will be most significant, should the COVID-19 and influenza epidemic overlap and peak around the same time during influenza season 2020/21. The majority of the population is still susceptible to COVID-19. Influenza and COVID-19 are difficult to distinguish based on clinical assessment[5]. A recent study[34]has shown that influenza vaccination coverage in Switzerland has decreased from 2012 to 2017. This decrease was also observed among those at the highest risk for influenza as well as COVID-19 (>65 years, chronically ill). Overall vaccine coverage among risk populations was 36.2% in 2017, well below the recommended WHO target.
We urgently recommend that strategies to increase the vaccination coverage for influenza are implemented for the upcoming influenza season. Strategies should target the risk groups for both influenza and COVID-19 as well as health care workers(Table 1).
Targeting children may reduce hospitalizations among adults who frequently contract influenza from children. However, this will be difficult to achieve in Switzerland in the short term. The general vaccination of children has never been recommended in our country, and the intranasal LAIV is not available. The NCS-TF believes that firm recommendations for vaccinating children cannot be made at this stage, but that the licensing of the intranasal vaccine in Switzerland would be highly desirable.
Expanding vaccine coverage requires multiple strategies:
- To expand influenza vaccination coverage,especially in high-risk groups, the government should implement a campaign with general and targeted information/communication focusing on solidarity and personal protection. This could be a cross-platform campaign,including newspapers, social media, and television,among others.-Strategies to increase vaccination coverage among health care workers should include
- Coverage of costs by the employer
- An educational program for staff
- Establishing a culture of prevention, for example with a “vaccine day”
- A campaign via e-mail, posters, employee newsletters etc.
- Action research using group discussion groups to understand why some staff is declining vaccination.
An important aspect is increasing access to influenza vaccination:
- The cost of the vaccination should be covered through the “obligatorische Krankenpflegeversicherung (OKP)”, with franchise exemption for patients at high risk and their contacts.
- Strategies to improve access to vaccination, such as the provision of vaccinations at pharmacies or mobile vaccine teams, as it is already in place in some places in Switzerland.
All strategies should integrate effective communication:
- Communication strategies should include general and setting-specific communication strategies (see also NCS-TF Policy brief communication and SARS-CoV-2 from July 2020).
Finally, we recommend strengthening other fundamental elements, such as non-pharmaceutical interventions (NPI), in the prevention of influenza transmission. Most of these interventions have already been promoted at the start and during the COVID-19 pandemic:
- Maintaining and strengthening hand hygiene,respiratory hygiene, including the wearing of masks
- Promotion ofsocial distancing as well as”test and stay home when sick”.
- The use of triple tests that detect SARS-CoV-2 as well as influenza A and B infections should be considered during the flu season.
Unresolved issues
Further studies are required to quantify the likely impact of influenza vaccination on the COVID-19 epidemic, and the comparative impact of NPIs on Covid-19 and influenza. Further studies are needed on the IFR of COVID-19 as well as the frequency and clinical impact of coinfections with influenza and other respiratory infections.
- Nicholson KG, Wood JM, Zambon M. Influenza. The Lancet 2003;362:1733–45. https://doi.org/10.1016/S0140-6736(03)14854-4
- Paules C, Subbarao K. Influenza. The Lancet 2017;390:697–708. https://doi.org/10.1016/S0140-6736(17)30129-0.
- Fauci AS, Touchette NA, Folkers GK. Emerging infectious diseases: a 10-year perspective from the National Institute of Allergy and Infectious Diseases. Emerg Infect Dis 2005;11:519–25. https://doi.org/10.3201/eid1104.041167.
- Bundesamt für Gesundheit. Impfen gegen Grippe. https://www.impfengegengrippe.ch/de-ch/die-grippe/gefaehrlich-saisonale-grippe.html (accessed September 6, 2020).
- Ozaras R, Cirpin R, Duran A, Duman H, Arslan O, Bakcan Y, et al. Influenza and COVID-19 coinfection: Report of six cases and review of the literature. J Med Virol https://doi.org/10.1002/jmv.26125.
- Belongia EA, Osterholm MT. COVID-19 and flu, a perfect storm. Science 2020;368:1163. https://doi.org/10.1126/science.abd2220.
- World Health Organization Office for Europe. Evaluation of seasonal influenza vaccination policies and coverage in the WHO European Region. Results from the 2008/2009 and 2009/2010 influenza seasons Based on a joint VENICE–ECDC–WHO survey. Copenhagen, Denmark: 2014.
- Bundesamt für Gesundheit. Neues Coronavirus: Besonders gefährdete Personen. https://www.bag.admin.ch/bag/de/home/krankheiten/ausbrueche-epidemien-pandemien/aktuelle-ausbrueche-epidemien/novel-cov/besonders-gefaehrdete-menschen.html (accessed September 6, 2020).
- Bundesamt für Gesundheit. Saisonale Grippe (Influenza). https://www.bag.admin.ch/bag/de/home/krankheiten/krankheiten-im-ueberblick/grippe.html (accessed September 6, 2020).
- KupferschmidtK. Why do some COVID-19 patients infect many others, whereas most don’t spread the virus at all? Science2020. https://www.sciencemag.org/news/2020/05/why-do-some-covid-19-patients-infect-many-others-whereas-most-don-t-spread-virus-all (accessed May 20, 2020).
- Lloyd-Smith JO, Schreiber SJ, Kopp PE, Getz WM. Superspreading and the effect of individual variation on disease emergence. Nature 2005;438:355–9. https://doi.org/10.1038/nature04153.
- Wong JY, Kelly H, Ip DKM, Wu JT, Leung GM, Cowling BJ. Case fatality risk of influenza A(H1N1pdm09): a systematic review. Epidemiol Camb Mass 2013;24. https://doi.org/10.1097/EDE.0b013e3182a67448.
- Meyerowitz-Katz G, Merone L. A systematic review and meta-analysis of published research data on COVID-19 infection-fatality rates. MedRxiv 2020:2020.05.03.20089854. https://doi.org/10.1101/2020.05.03.20089854.
- Furukawa NW, Brooks JT, Sobel J. Evidence Supporting Transmission of Severe Acute Respiratory Syndrome Coronavirus 2 While Presymptomatic or Asymptomatic. Emerg Infect Dis 2020;26. https://doi.org/10.3201/eid2607.201595.
- Ludvigsson JF. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr Oslo Nor 1992 2020;109:1088–95. https://doi.org/10.1111/apa.15270.
- Morand A, Fabre A, Minodier P, Boutin A, Vanel N, Bosdure E, et al. COVID-19 virus and children: What do we know? Arch Pédiatrie 2020;27:117–8. https://doi.org/10.1016/j.arcped.2020.03.001.
- Munro A, Roland D. The missing link? Children and transmission of SARS-CoV-2. Dont Forget The Bubbles 2020. https://doi.org/10.31440/DFTB.25585.
- Götzinger F, Santiago-García B, Noguera-Julián A, Lanaspa M, Lancella L, Calò Carducci FI, et al. COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. Lancet Child Adolesc Health 2020;4:653–61. https://doi.org/10.1016/S2352-4642(20)30177-2.
- Glezen WP, Couch RB. Interpandemic influenza in the Houston area, 1974-76. N Engl J Med 1978;298:587–92. https://doi.org/10.1056/NEJM197803162981103.
- Shang M, Blanton L, Brammer L, Olsen SJ, Fry AM. Influenza-Associated Pediatric Deaths in the United States, 2010-2016. Pediatrics 2018;141. https://doi.org/10.1542/peds.2017-2918.
- Basurto-Dávila R, Meltzer MI, Mills DA, Beeler Asay GR, Cho B-H, Graitcer SB, et al. School-Based Influenza Vaccination: Health and Economic Impact of Maine’s 2009 Influenza Vaccination Program. Health Serv Res 2017;52 Suppl 2:2307–30. https://doi.org/10.1111/1475-6773.12786.
- Fiore AE, Epperson S, Perrotta D, Bernstein H, Neuzil K. Expanding the recommendationsfor annual influenza vaccination to school-age children in the United States. Pediatrics 2012;129 Suppl 2:S54-62. https://doi.org/10.1542/peds.2011-0737C.
- Kassianos G, MacDonald P, Aloysius I, Reynolds A. Implementation of the United Kingdom’s childhood influenza national vaccination programme: A review of clinical impact and lessons learned over six influenza seasons. Vaccine 2020;38:5747–58. https://doi.org/10.1016/j.vaccine.2020.06.065.
- Pebody RG, Green HK, Andrews N, Boddington NL, Zhao H, Yonova I, et al. Uptake and impact of vaccinating school age children against influenza during a season with circulation of drifted influenza A and B strains, England, 2014/15. Eurosurveillance 2015;20:30029. https://doi.org/10.2807/1560-7917.ES.2015.20.39.30029.
- Bundesamt für Gesundheit. DIE SAISONALE GRIPPEIMPFUNG WIRD EMPFOHLEN FÜR: 2017. https://www.bag.admin.ch/dam/bag/de/dokumente/mt/infektionskrankheiten/grippe/empfehlung-grippeimpfung-kurz.pdf.download.pdf/empfehlungen-grippeimpfung-kurz-de.pdf.
- Talbot HK, Zhu Y, Chen Q, Williams JV, Thompson MG, Griffin MR. Effectiveness of influenza vaccine for preventing laboratory-confirmed influenza hospitalizations in adults, 2011-2012 influenza season. Clin Infect Dis Off Publ Infect Dis Soc Am 2013;56:1774–7. https://doi.org/10.1093/cid/cit124.
- Pereira M, Williams S, Restrick L, Cullinan P, Hopkinson NS, London Respiratory Network. Healthcare worker influenza vaccination and sickness absence -an ecological study. Clin Med Lond Engl 2017;17:484–9.https://doi.org/10.7861/clinmedicine.17-6-484.
- Phrommintikul A, Kuanprasert S, Wongcharoen W, Kanjanavanit R, Chaiwarith R, Sukonthasarn A. Influenza vaccination reduces cardiovascular events in patients with acute coronary syndrome. Eur Heart J 2011;32:1730–5. https://doi.org/10.1093/eurheartj/ehr004.
- Colquhoun AJ, Nicholson KG, Botha JL, Raymond NT. Effectiveness of influenza vaccine in reducing hospital admissions in people with diabetes. Epidemiol Infect 1997;119:335–41. https://doi.org/10.1017/s095026889700825x.
- Liu W-C, Lin C-S, Yeh C-C, Wu H-Y, Lee Y-J, Chung C-L, et al. Effect of Influenza Vaccination Against Postoperative Pneumonia and Mortality for Geriatric Patients Receiving Major Surgery: A Nationwide Matched Study. J Infect Dis 2018;217:816–26. https://doi.org/10.1093/infdis/jix616.
- Arriola CS, Anderson EJ, Baumbach J, Bennett N, Bohm S, Hill M, et al. Does Influenza Vaccination Modify Influenza Severity? Data on Older Adults Hospitalized With Influenza During the 2012-2013 Season in the United States. J Infect Dis 2015;212:1200–8. https://doi.org/10.1093/infdis/jiv200.
- Ferdinands JM, Olsho LEW, Agan AA, Bhat N, Sullivan RM, Hall M, et al. Effectiveness of influenza vaccine against life-threatening RT-PCR-confirmed influenza illness in US children, 2010-2012. J Infect Dis 2014;210:674–83. https://doi.org/10.1093/infdis/jiu185.
- Mosby LG, Rasmussen SA, Jamieson DJ. 2009 pandemic influenza A (H1N1) in pregnancy: a systematic review of the literature. Am J Obstet Gynecol2011;205:10–8. https://doi.org/10.1016/j.ajog.2010.12.033.
- Zuercher K, Zwahlen M, Berlin C, Egger M, Fenner L. Losing ground at the wrong time: Trends in self-reported influenza vaccination uptake in Switzerland, Health Survey 2007-2017. MedRxiv 2020:2020.06.05.20123026. https://doi.org/10.1101/2020.06.05.20123026.
- Stringhini S, Wisniak A, Piumatti G, Azman AS, Lauer SA, Baysson H, et al. Seroprevalence of anti-SARS-CoV-2 IgG antibodies in Geneva, Switzerland (SEROCoV-POP): a population-based study. Lancet Lond Engl 2020;396:313–9. https://doi.org/10.1016/S0140-6736(20)31304-0.
- Li Q, Tang B, Bragazzi NL, Xiao Y, Wu J. Modeling the impact of mass influenza vaccination and public health interventions on COVID-19 epidemics with limited detectioncapability. Math Biosci 2020;325:108378. https://doi.org/10.1016/j.mbs.2020.108378.
- Scott S. Flu deaths drop in Australia as coronavirus restrictions save hundreds of lives 2020. https://www.abc.net.au/news/2020-07-23/coronavirus-restrictions-cause-flu-cases-to-drop-australia/12480190 (accessed September 6, 2020).
- Chow A, Hein AA, Kyaw WM. Unintended Consequence: Influenza plunges with public health response to COVID-19 in Singapore. J Infect 2020;81:E68–9. https://doi.org/10.1016/j.jinf.2020.04.035
Date of request: 15/7/2020
Date of response: 26/9/2020
In response to request from: GDK
Comment on planned updates: Update planned as soon as an important body of new evidence becomes available.
Expert groups involved: Matthias Egger,
Claire-Ann Siegrist with the help of staff at ISPM Bern (Kathrin Zürcher, Catrina Mugglin), Public Health Group (Marcel Tanner), Christoph Berger, Kinderspital Zürich
Contact person: Matthias Egger