– Policy Brief
Summary of request
To evaluate the epidemiological risk (more specifically, the post-quarantine transmission risk) for different strategies of quarantining after contact tracing.
Executive summary
Currently, individuals who have been in close contact with a confirmed SARS-CoV-2 case are obliged to go into quarantine until 10 days after the presumed last exposure (here referred to as strategy 0). The Science Task Force has been asked by the BAG/EDI to assess the effect of quarantine duration of three alternative strategies for the quarantine of contacts,all based on the test and release principle Strategy 1 is a test & release strategy with testing on day 7 and release if the test result is negative. Strategy 2 is based on two tests, one at the day when the individual is contacted and one on day 7, and the individual is released on day 7 if both tests are negative. Strategy 3 is based on tests on days 5 and 7, and releases individuals on day 5 when the test is negative, with the obligation to test again on day 7. For all strategies, released individuals are required to minimize contacts and wear masks outside home at all times until day 10 after presumed exposure. We assume here that these preventive measures result in a reduction of transmission by 50% for any individual released early due to a false negative test.
We find that strategies 1 and 2 perform marginally worse than the currently implemented strategy 0 based on 10 day quarantine (see figure 1). In terms of preventing onward transmission from quarantined individuals, there is only little gain by testing the quarantined individual at the time when s/he is contacted which is the only difference between strategy 2 and strategy 1. However, an epidemiological benefit of strategy 2 over strategy 1 is expected due to the early detection of further confirmed cases and the tracing of their contacts. However, this benefit is related to the identification of index cases for further contact tracing and is not related to the duration of quarantine.
Strategy 3 (serial testing) performs significantly worse than all other strategies (see figure 1). This is due to the substantial expected false negative rate of individuals tested 5 days after presumed exposure. Individuals released from quarantine after a false negative test at day 5 are then at the presumed peak of infectivity. They may transmit for two days even if the subsequent test at day 7 then turns out to be positive.
Any shortening of the duration of quarantine will increase overall transmission unless the extra transmission resulting from shortening of quarantine would be overcompensated by better adherence. At the current situation with high case numbers, overburdened hospitals as well as the risk of the spread of new, more transmissible variants shortening quarantine should only be considered if other measures are implemented to compensate for its presumed effects on increasing transmission.
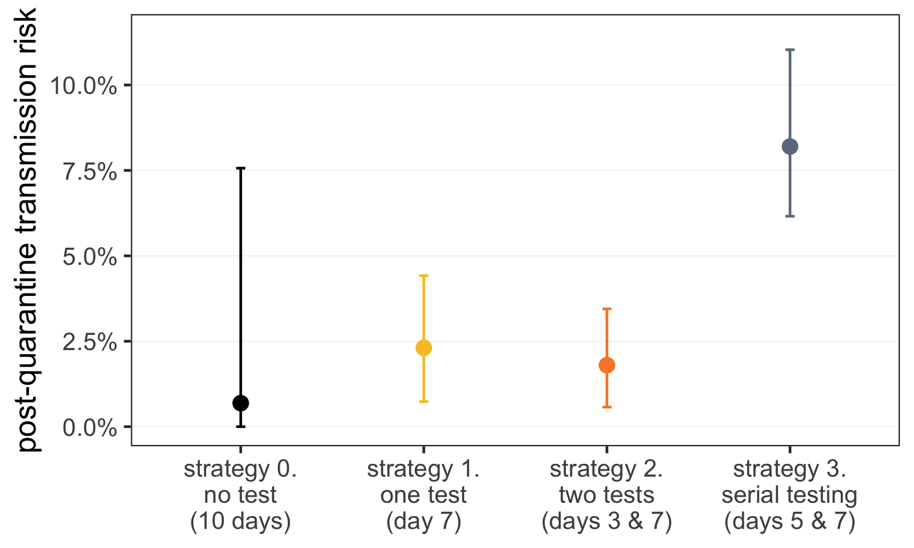
Figure 1: The post-quarantine transmission risk, i.e. the percentage of the total transmission potential that remains after quarantine is completed, under four quarantine strategies. Individuals are infected with SARS-CoV-2 at time tE=0. They enter quarantine at time tQ=3. Under the currently implemented strategy 0, they are released on day tR=10 without any tests. Under strategy 1 they are tested on day tT=7, and released on day tR=7 if the result is negative. Under strategy 2 the infected individual is tested on quarantine entry (here on day tQ=3) and then tested again on day tT=7. They are released on day tR=7 only if both tests are negative. Under strategy 3 the infected individuals are tested on day tT1=5 and released immediately if the test is negative. They are tested again on day tT2=7, and if negative they are released on day tR=7. We assume that the rapid antigen test has the same false negative rate as reported by Kucirka et al. (2020) for the RT-PCR based tests. Moreover we assume that all transmission between day of release and day 10 is reduced by 50% due to minimizing contacts and wearing of masks outside home at all times until day 10 after presumed exposure. Error bars reflect the uncertainty in the generation time distribution as given by Ferretti et al. (2020).
Main text
Description of alternative strategies
We have been requested by BAG/EDI to look at three alternative strategies to the currently implemented quarantine of contacts. These strategies are described below and the original German text as received from Céline Gardiol, BAG, is given in Appendix 1. The rationale for alternative strategies is to use testing to shorten the duration of quarantine.
Strategy 1 is a test and release strategy with testing on day 7. The contact persons go into quarantine for 10 days from the last contact with the infected person (if the person does not live in the same household) or from the day on which the infected person was isolated (if the person lives in the same household). The quarantine is lifted if the affected person performs a rapid antigen test or PCR test from the 7th day after the last contact and this shows a negative result. In order to limit the residual risk of infection, the person concerned should be advised to limit contact with other people during the three days following the test and to always wear a mask when out of the house.
Strategy 2 is a test and release strategy with testing on the day when the person is informed to go into quarantine and on day 7. The contact persons go into quarantine for 10 days from the last contact with the infected person (if the person does not live in the same household) or from the day on which the infected person was isolated (if the person lives in the same household). The quarantine is lifted if the person concerned performs a rapid antigen test or PCR test both on the day on which contact is made by the responsible cantonal authority and from the 7th day after the last contact, and both tests indicate a negative result. In order to limit the residual risk of infection, the person concerned should be advised to limit his or her contacts with other people during the three days following the second test and to always wear a mask when out of the house.
Strategy 3 is referred to as the replacement of quarantine by serial testing. Quarantine can be shortened if two tests are required after the last contact with the infected person. The person in quarantine is required to be tested for the first time 5 days after the last contact with the infected person. If the test result of this first test is negative, the quarantine does not have to be continued. However, because a relatively large number of people still develop symptoms after the 5th day, release on the 5th day can only be justified from an epidemiological point of view if the person concerned takes another test on the 7th day. In addition, until the 10th day contacts should be kept to a minimum and a mask should always be worn outside the home.
For comparison we include the currently implemented strategy which is to quarantine persons for 10 days after the last close contact with a confirmed case (link). This strategy is referred to here as strategy 0.
Assumptions underlying the calculation of th effect on transmission
- Strategies 1-3 all aim to reduce the residual risk of transmission after early release from quarantine by advising to keep contacts to a minimum and wear masks when outside the home until 10 days after the presumed last exposure. It is unclear by how much this may reduce any residual transmission. Here we assume that this reduces the residual transmission by 50%.
- We assume throughout that individuals who have been in close contact with an infected case are put into quarantine 3 days after the exposure (i.e. tQ=3)
- We use for the false negative rate of PCR tests as a function of the days since exposure the estimates published by Kucirka et al. (2020), which are based on the detection of SARS-CoV2 by RT-PCR amongst people who developed symptoms. For lack of information we assume that the false negative rate of the rapid antigen tests is equal to that of the PCR tests.
- To estimate the effect of the different strategies for quarantine of contacts we follow the method as described in Ashcroft et al. (2020). This study presents a mathematical model that allows quantification of the effects of changing quarantine duration based on the distributions of incubation time (time from infection to onset of symptoms), infectivity (infectiousness as a function of days since symptom onset), and generation time (difference of time points of infection between infector and infectee) that have been described by Ferretti et al. (2020).
Results: Assessment and comparison of strategies
The post-quarantine transmission risk of infected individuals for the four different strategies is shown in figure 1. Strategies 1 and 2 have only a marginally increased post-quarantine transmission risk relative to the currently implemented strategy 0. Strategy 3 however is significantly worse than all other strategies. Figure 2 shows the post-quarantine transmission risk that remains after quarantine is completed under strategy 0 and strategy 1 as a function of release date.
As pointed out in an earlier policy brief by the Science Task Force, this strategy 1 poses a low risk of additional new infections compared to the currently implemented strategy 0, but offers the benefit of releasing individuals 3 days earlier from quarantine if the test result on day 7 is negative.
Strategy 2 differs from strategy 1 in testing quarantined individuals also at the time when they are contacted. This results only in a small gain in terms of preventing transmission from the quarantined individuals as in both strategies individuals remain in quarantine until day 7. However, an epidemiological benefit of strategy 2 over strategy 1 is expected arising from the early detection of further confirmed cases and the subsequent tracing of their contacts. However, this benefit is not related to the duration of quarantine. This secondary effect will depend on when contacts are quarantined relative to their exposure. If they are quarantined soon after exposure (<3 days), then they have both a low probability to have already transmitted further before being put into quarantine and also a low probability that their test will turn out to be positive. In both cases the test will not offer a substantial benefit to breaking transmission chains by contact tracing. Should individuals be quarantined more than 3 days after exposure then if they are indeed infected the chance that they have already transmitted increases substantially. In this case testing quarantined individuals offers a benefit to breaking transmission chains if their contacts are identified by contact tracing. We agree with the point raised in the assessment by the BAG (see German text further below), that individuals obtaining a negative test result from the first test may have reduced motivation to adhere to quarantine. This would be an unwanted negative side effect of testing individuals at the time when they are contacted.
Strategy 3 is substantially worse than both considered alternatives (strategy 1 and 2) as well as the currently implemented system in terms of preventing onward transmission from quarantined individuals. The reason is that a test 5 days after presumed exposure carries a substantial risk of a false negative result. In this case an infected individual is not only erroneously released, but also at a time when infectivity is at the peak. A second test at day 7 may correct such an earlier erroneous result, but nevertheless substantial transmission has already occurred between days 5 and 7. Note that we do not consider in our estimates that people who have tested negative on day 5 may not return for the test on day 7. A lack of adherence to the second test would result in further transmission.
Note also, that we assume for strategies 1-3, that persons released early from quarantine adhere to the request to minimize contacts and wear masks outside home at all times. We assume that this results in a 50% reduction of transmission from people between days. Moreover we assume that there is no difference in adherence to this request between the different strategies.
As has been pointed out by the Science Task Force before (policy brief), the reduction of the duration of quarantine needs to be assessed in the context of the overall epidemiological situation. Any shortening of the duration of quarantine will increase overall transmission unless the extra transmission resulting from shortening of quarantine would be overcompensated by better adherence. At the current situation with high case numbers, overburdened hospitals as well as the risk of the spread of new, more transmissible variants shortening quarantine should only be considered if other measures are implemented to compensate for its presumed effects on increasing transmission.
Note, that the presented estimates for the post-quarantine transmission risk are based on data that was obtained prior to the appearance of the new, more transmissible variants from the UK and South Africa. To date it is not known whether the peak or duration of infectiousness in persons infected with these new variants differ from those used for the current estimates of the infectiousness profile. If the increased transmissibility was in part due to a longer infectiousness period, then estimates presented here do not apply to the new variants, and the question of quarantine duration needs to be revisited, at the very least for those individuals in contact with infected individuals carrying these strains. The new variants pose further challenges for testing and diagnosis that are independent of the questions concerning quarantine duration, as the differential diagnosis of infection with the new variants is more complex and slower.
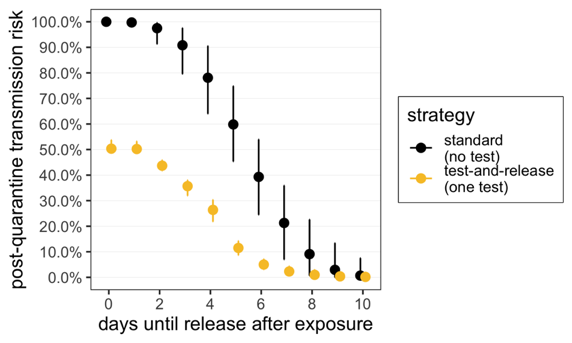
Figure 2: The post-quarantine transmission risk that remains after quarantine is completed under standard (no test) and test-and-release (one test) quarantine as a function of release date. An individual is infected with SARS-CoV-2 at time tE=0. We assume that testing and release occur on the same day (i.e. a rapid test). For test-and-release, transmission before day 10 is reduced by 50% due to reinforced hygiene measures. Error bars reflect the uncertainty in the generation time distribution.
Methods
Model description
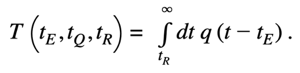
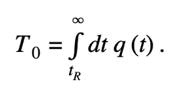
The timing of onward transmission from an infected individual is determined by the generation time distribution, q(t), which describes the time interval between the infection of an infector and infectee. To quantify the risk of transmission occurring after release from quarantine, we need to know the time at which the individual was exposed (tE), as well as when they enter (tQ) and are released from (tR) quarantine. The fraction of transmission that occurs post-quarantine is then the total transmission probability (i.e. the area under the curve) that occurs after tR:
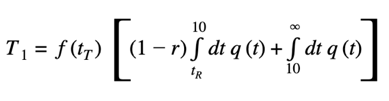
The test-and-release strategy uses virological testing during quarantine to release individuals with a negative test result and to place those with a positive test result into isolation. A test is issued at time tT ≥ tQ. If the test is negative, the individual is released when the test result arrives at time tR. Otherwise, the individual is isolated until they are no longer infectious. One challenge with this strategy is the high probability of a false-negative RT-PCR test result (i.e. an infected individual is prematurely released into the community) (Kucirka et al. 2020). The fraction of transmission that occurs after an early release from quarantine under the test-and-release strategy is:
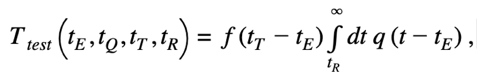
where the function f(t) is the false-negative probability at time t after infection as described in Kucirka et al. (2020).
Strategy 0: Baseline quarantine
The contact persons go into quarantine for 10 days from the last contact with the infected person (if the person does not live in the same household) or from the day on which the infected person was isolated (if the person lives in the same household).
Calculation: We fix the exposure time to tE = 0. The fraction of transmission that occurs post-quarantine, if released on day tR, is
Strategy 1: Test-and-release strategy with testing on day seven
The contact persons go into quarantine for 10 days from the last contact with the infected person (if the person does not live in the same household) or from the day on which the infected person was isolated (if the person lives in the same household). The quarantine is lifted if the affected person performs a rapid antigen test or RT-PCR test from the seventh day after the last contact and this shows a negative result. In order to limit the existing residual risk of infection, the person concerned should be advised to limit their contacts with other people in the three days following the test and to always wear a mask when out of the house.
Calculation: If a positive test result is returned, then that individual is isolated until they are no longer infectious, resulting in no post-quarantine transmission. A false-negative test result, for a test taken on day tT, occurs with probability f(tT). These individuals are released on day tR, but remain infectious. Transmission is reduced until day 10 by a factor (1 – r), where r is the fraction of transmission prevented by reinforced hygiene rules. After day 10, any residual transmission occurs at full strength. the fraction of transmission that occurs post-quarantine is then
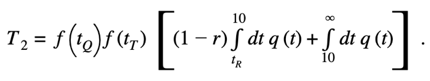
Strategy 2: Test-and-release strategy with testing on the day of contact and on day seven
The contact persons go into quarantine for 10 days from the last contact with the infected person (if the person does not live in the same household) or from the day on which the infected person was isolated (if the person lives in the same household). The quarantine is lifted if the person concerned performs a rapid antigen test or PCR test both on the day on which contact is made by the competent cantonal authority and from the seventh day after the last contact, and both tests indicate a negative result. In order to limit the residual risk of infection, the affected person should be advised to limit contact with other people during the three days following the second test and to always wear a mask outside the home.
The first test allows identification of asymptomatic persons infected with SARS-CoV-2. In case of a positive result of the first test, any close contacts of the person in contact quarantine can also be quarantined as soon as possible. In this way, chains of transmission can be efficiently interrupted. A negative result of the first test does not end the quarantine prematurely; the person concerned has to comply with the quarantine until the next test from the 7th day after the last contact with the case.
Calculation: Individuals are tested at time tQ (i.e. upon quarantine entry) and time tT. Any positive result ensures this individual is isolated until they are no longer infectious, and they do not contribute to post-quarantine transmission. Only individuals who return two negative test results are released early from quarantine and contribute to transmission.
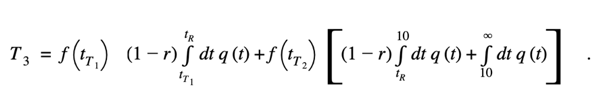
Strategy 3: Replacement of quarantine by serial testing
Quarantine can be further shortened because two tests are required after the last contact with the infected person. The person in quarantine is required to be tested for the first time 5 days after the last contact with the infected person. If the test result of this first test is negative, the quarantine does not have to be continued. However, because a relatively large number of people still develop symptoms after the fifth day, release on the fifth day can only be justified from an epidemiological point of view if the person concerned takes another test on the seventh day. In addition, contacts until the 10th day should be kept to a minimum and a mask should always be worn outside the home.
Calculation: Individuals who receive a false-negative test result after the first test at time tT1 will contribute to transmission until tR. A second false-negative result will lead to extra transmission from tR until t→∞. Any positive test will remove the individual from the infectious pool and prevent further transmission
References
Ashcroft, P., Lehtinen, S., Angst, D. C., Low, N., & Bonhoeffer, S. (2020). Quantifying the Impact of Quarantine Duration on COVID-19 Transmission. medRxiv, https://doi.org/10.1101/2020.09.24.20201061.
Ferretti, L., et al. (2020). The Timing of COVID-19 Transmission. medRxiv, https://doi.org/10.1101/2020.09.04.20188516.
Kucirka, L. M., Lauer, S. A., Laeyendecker, O., Boon, D., & Lessler, J. (2020). Variation in False-Negative Rate of Reverse Transcriptase Polymerase Chain Reaction–Based SARS-CoV-2 Tests by Time since Exposure. Annals of Internal Medicine, 173(4), 262–267, https://doi.org/10.7326/M20-1495.
Type of document: Modelling Study
In response to request from: BAG/EDI
Date of request: 22/12/2020
Date of response: 04/01/2021
Experts involved: Peter Ashcroft and Sebastian Bonhoeffer
Contact persons: Sebastian Bonhoeffer