Download PDF
This situation report focuses on:
- The current situation of the health care system in Switzerland,
- Factors that affect adherence and compliance to the measures that are currently in place,
- Preparations and actions needed in the healthcare system,
- On when we expect to find out whether the measures to stop the spread of the epidemic are effective.
1. General overview of the situation, outlook of reaching capacity limits in the healthcare system
Since the beginning of October 2020, the daily number of positive SARS-CoV-2 tests, hospitalizations, ICU admissions and deaths are doubling approximately weekly. As a consequence, we expect that critical limits of our healthcare system will be reached between the 8th and 18th of November, based on the predictions of October 29th. Here, we discuss limits in the capacity of hospital wards and intensive care units based on the available data.
Hospital beds: As reported in the Informations- und Einsatz-System of the Koordinierter Sanitätsdienst, there are over 24’300 hospital beds available in Switzerland, of which about 6’000 beds are currently free. If the number of hospitalizations increased at the current level, the limits of the capacity could be reached soon.
ICU beds: Figure 1 shows the current prediction of the number of ICU beds that will be occupied, and the time until the limits of the capacity will be reached.
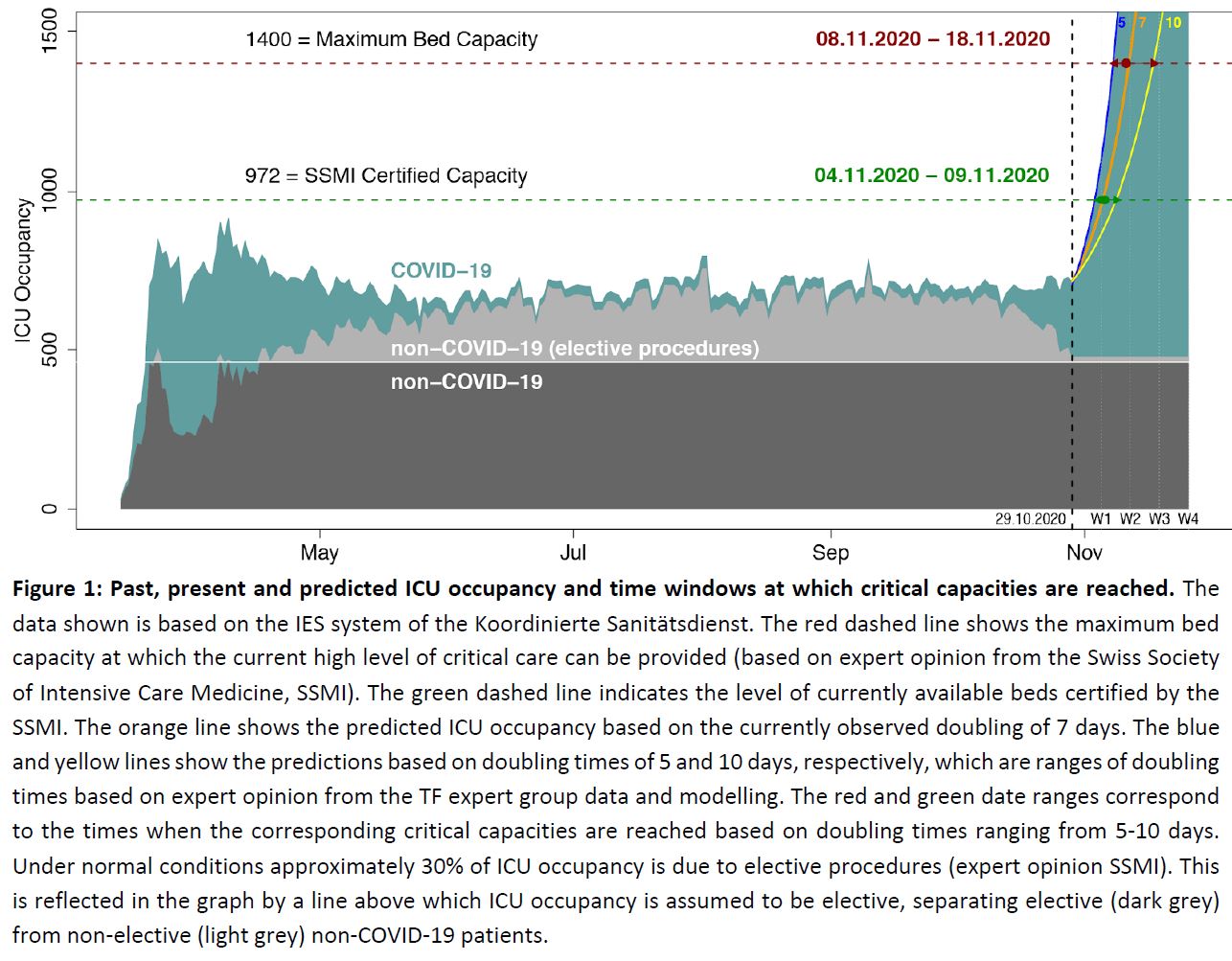
There is therefore a high risk of Switzerland reaching and then exceeding the capacity of hospital beds and ICU beds between the 8th and 18th of November, based on the predictions of October 29th. Such a situation would compromise care for COVID-19 and non-COVID-19 patients alike. As discussed below – while we expect that the measures taken on a cantonal and national level in October 2020 will improve the situation, there is a substantial probability that their effect will manifest after the limits of the healthcare system have been reached or exceeded.
Even if the risk of reaching and exceeding the limits of the healthcare system is imminent, it is, of course, extremely important to reduce the extent and the duration of capacity overflow. Reducing the extent and the duration means that fewer patients will be in a situation where standard-of-care cannot be maintained.
It is important to note that this situation – an overflow of the capacity of the health care system – can fundamentally only be solved by strongly reducing the transmission of SARS-CoV-2 and thereby decreasing the number of COVID-19 patients. Increases in the capacity of the health care system can mitigate the situation in the short term, but does not offer a sustainable solution. This is because, without stopping the spread of SARS-CoV-2, any capacity increase would rapidly be offset by an increase in case numbers. Strictly as an example, if it was possible to add 200 fully staffed ICU beds, then, at a doubling time of one week, this would delay the moment when the limits of the capacity are reached by less than two days.
2. What needs to be done so that the measures are effective?
In October 2020, a number of national and cantonal measures were taken. The goal of these measures is to reverse the trend described above and achieve a reduction in case numbers, hospitalizations and deaths. Here we discuss the factors that determine the effectiveness of these measures.
The key determinants to achieve a high degree of effectiveness of the combination of measures that have been put in place are timeliness as well as:
- Compliance by all stakeholders and the providers of the health and social services
- Adherence of the people, decision makers and stakeholders to the measures in a spirit of solidarity and joint responsibility
Compliance and adherence are of particular importance in a situation where the interventions aim at protecting the health care system while also protecting the economy, social life, freedom and access to education.
Consequently the implementation of measures need to be well understood by the whole population. Clear communication is key. Communication should range from general to targeted, focused on different target and risk groups while respecting the social, cultural and economic diversity of our country. Major communication efforts have to be mounted swiftly but with a long-term perspective. Key messages should aim at (i) providing or creating understanding for the measures, (ii) providing very practical outlooks on how individuals, families, teams, companies can still pursue and also enjoy social and economic activities within the boundaries of the measures and thus (iii) provide an outlook towards normality. Compliance and adherence is always increased when positive outlooks are generated. Creating fear has short-lived and mostly negative effects on compliance and adherence as shown in numerous studies in public health and social science.
Mix-methods polls, surveys, and observations should be requested on an ongoing basis to understand the behavior of the population in near-real time. Such information should be used to refine and improve the overall response strategy in terms of acceptance of measures and recommended behaviors, but also the way in which they are communicated to each stakeholder group. For example, the measure may be accepted, but people might not know what or how to adhere (thus a change in communication design or delivery would be required). Alternatively, a measure might not be accepted even though communicated well. In this case, the measure may need to be justified more clearly or refined so that people accept it. Monitoring and refining must be an ongoing process for the duration of the pandemic especially as people become tired of the situation or fail to see direct benefits of their actions.
3. What preparations and actions are needed in the healthcare system?
A number of preparations and actions in the healthcare system are critical which are beyond the scope of the Science Task Force. In this paragraph we highlight aspects which are at the interface of implementation science and implementation. These include, but are not limited to, advance care planning, triage of patients, dealing with long term effects of COVID-19, support for HCW and other essential workers, families, as well as those with non COVID-19 related health problems.
Advance care planning should be made widely available throughout primary care and requires support. It is an essential part of respect for the right of patients to self-determination, and improves care through patient participation in their health management. At this time, when the risk of developing a severe disease is increased by the possibility of contracting COVID19, it is particularly important to promote this possibility to respect patients’ wishes, and also to avoid imposing intensive therapies on those who do not wish them. This is also important for an appropriate management of intensive care resources; for this reason, the SAMW-SGI guidelines on “Triage for intensive-care treatment under resource scarcity” issued in March 2020 also emphasize the importance of discussing end of life wishes with relatives and healthcare teams, so that when the time comes, wishes are know. Persons at every stage of life who wish to discuss their priorities in case of a severe case of COVID19 with their families, express these priorities in an advance directive, and name a proxy in case they become incapable of decision-making, can need support in doing so. Providing primary care physicians and other health care providers who provide such support with the required resources, including relevant information, would facilitate this.
Specific guidelines for the triage of patients in case of limited resources in intensive care have been updated in a collaborative work by the SAMW and SGI. These guidelines, which will be published in the upcoming days, provide indications for ICU admission and management, as an annexe to the SAMW 2013 medico-ethical guidelines on “Intensive care interventions” .There are no COVID-specific guidelines for the triage at hospital admission, or guidelines for the orientation of nursing home residents. In such cases, general medico-ethical guidelines of the SAMW are the reference documents.
- Rehabilitation will be necessary for many patients after Covid-19, not only for ICU patients. It is important to build up capacity for rehabilitation and clarify the financing of rehabilitation.
- More implication of the primary care healthcare workers (primary care physicians, nurses, physiotherapist), who are in contact with the majority of infected patients, who are not hospitalized, but nevertheless have questions and need reassurance and advice.
- We expect pressure on mental health care and promotion (including prevention) capacity and psychiatric care in the coming months, and we need to build up capacity.
- As happened in the spring of 2020, there is a danger that chronic patients and acute non-COVID patients will stay at home because of fear of getting infected. After the period in spring, there were many patients with long-term exacerbations of chronic diseases that were not managed for months, and with severe consequences of acute diseases that were not treated. It is important to avoid this situation in the future.
4. Protecting the health care system: what parameters need to be observed, and what decisions are coming up?
The recent rapid increases of infections and hospitalizations are expected to lead to Switzerland reaching limits of the health care system in a very short time frame. The measures that have been put in place in October aim at reversing this trend. Here, we focus on scientific aspects, i.e. how we can analyze whether these measures are successful, and discuss how quickly we can expect to see evidence for effectiveness.
The main question is whether the measures in Switzerland are successful in leading to a reduction in the number of new positive tests, hospitalizations, ICU admissions and deaths per day. There are indirect indicators that can offer first insights into the effect of measures on travel, mobility, home office activity, and more. These indicators are valuable and can potentially reveal with almost no time delay whether implemented measures show an effect. However, since these measures are indirect, it remains to be established whether these indicators can reliably predict whether a reduction of case numbers will be achieved. To do so, one needs to monitor the development of positive tests, hospitalizations, ICU admissions and deaths
There are time delays between the moment when new measures are imposed and the time when the effects of these measures are visible in the population. This is because of the time that elapses from a person being infected until this person develops symptoms, gets tested and possibly gets admitted to the hospital. Here, we discuss these time delays, and compare them to the dynamics at which Switzerland is approaching the capacity limits of the health care system.
There are four indicator variables that are routinely collected: (i) the daily number of new confirmed cases and the percentage of positive tests, (ii) the daily number of newly hospitalised patients (iii) the daily number of patients on ICU and (iv) the daily number of deaths. All these numbers are taken from the FOPH obligatory notification data, except the ICU patients, which are taken from the IES system. Of these numbers the most relevant one is currently the number of patients on ICU, because this number is currently least affected from reporting delays and potential biases.
Measures implemented today and thus reducing transmission today will become manifest in any of the above indicator variables only with a substantial time delay. The mean time delays are: (i) 8 days from infection to the confirmation of a case (more specifically, assuming a mean of five days until onset of symptoms and a mean of 3 days from symptoms to a positive test), (ii) 9.5 days from infection to hospitalisation, (iii) 12 days from infection to ICU and (iv) 17 days from infection to death. These time delays are estimates based on the data from the obligatory notification data by the FOPH. Added to these time delays are delays in reporting that affect in particular the data from the obligatory notification (and less the data on ICU patients from the IES system). In reality the time delays may be even longer, because in spring the time from the implementation of strong measures on March 17 to peak occupancy in ICU ranged between 2-3 weeks (e.g. CHUV 22 days, HUG 14 days, Insel Bern 23 days).
The number of confirmed cases should therefore first reveal an effect of the measures. However, this number is directly affected by test availability and accessibility (which patients get tested); an increase in test positivity (the fraction of positive test per test performed) can be indicative of reduced availability or accessibility. A decrease in daily number of new positive cases needs thus to be interpreted with caution and may not be indicative of the measures showing first effects. Also this number regularly shows intermittent decreases due to reduced testing on weekends.
The number of hospitalised cases is less affected by biases (such as testing), but currently there are substantial delays in the reporting of hospitalisation (which was confirmed in a meeting between the Science Task Force and the BAG on 27.10.2020). Therefore a decrease in hospitalisation towards the most recent time cannot be taken as a sign of the spread of the epidemic slowing down.
The number of patients requiring intensive care is currently least affected by biases and is most reliably updated (and taken from the IES system). Moreover, it is the number that is most directly linked to the ability to maintain critical medical infrastructure.
The daily number of deaths also suffers less from biases then the daily number of confirmed cases. However, this number shows the longest delay before measures take effect. Also it is the lowest number, and therefore most affected by stochasticity, which makes it less reliable to deduce trends.
It is important to note that at least one week of data is required to allow the reliable detection of a trend change. Hence, basing the assessment of a trend change on the number of patients requiring ICU implies that we need from the day when new measures are implemented 12 days (due to the time delay) plus 7 days (to detect a trend change). For this reason, we expect to be able to assess whether a trend has been achieved with sufficient certainty at best only 19 days after the implementation of the measures.
For the measures imposed at the national level on October 29, we therefore expect to know their effect with some degree of certainty on November 17. Individual cantons took comparable measures at an earlier time point that are comparable to the national measures imposed on October 29. The canton of Valais took such measures on October 21, and we expect to be able to evaluate their effect with some certainty around November 9.
It is important to keep in mind that, if additional measures are taken at these time points (e.g. on November 9 or 17), then it will again take 12 days until these measures would start to have an effect in terms of reducing ICU hospitalization.
With the current ICU occupancy (227 cases based on database query on 28.10.2020 at 17:26) and the current doubling time (7 days) the expected number of patients requiring ICU hospitalisation is around 1450 in two weeks (on November 12) and thus already beyond the estimated capacity of beds (1400 beds) at which the current high quality of ICU care can be maintained (see Figure 1). With a range of doubling times from 5-10 days, that 1400 ICU bed limit is expected to be reached between the 7th and the 17th of November. Moreover the graph shows that in recent times elective procedures have already decreased, demonstrating that already at present the increase in COVID-19 ICU patients affects the health care in Switzerland.
