14 September 2020 – Policy Brief
Executive summary
Switzerland is pursuing a strategy that aims to contain the spread of SARS-CoV-2. The goal of this containment strategy is to keep numbers of infected people, hospitalisations, and deaths low until effective vaccine and treatment strategies become widely available. This strategy aims at finding a combination of control measures that allows containing the epidemic while protecting the economy and the freedom of individuals to the largest degree possible, and to continously improve this approach based on new evidence that becomes available.
Some have proposed that containment measures should be relaxed so that a large proportion of the population is infected with SARS-CoV-2 and might become immune to the virus. This policy brief shows that this approach would cause widespread damage to health, society and the economy, for the following reasons:
- It is not clear to what degree people who have been infected by SARS-CoV-2 are immune to future SARS-CoV-2 infections, and for how long immunity would last. Mild infections in particular might not lead to substantial protective immunity.
- Widespread infection in the population will lead to high numbers of severe disease outcomes and deaths. When case numbers go up, it is increasingly difficult to prevent the spread of infection to vulnerable groups.
- COVID-19 can result in prolonged health problems, even among persons with milder acute disease.
- Letting large parts of the population get infected, without overwhelming the healthcare system would take a very long time, in the range of 1-2 years.
- When case numbers are high, testing and contact tracing capacity will become overwhelmed and outbreak control will become more difficult. More restrictive and costly measures to control the epidemic would have to be imposed. These measures are economically much more damaging than contact tracing and are more restrictive for society. Long periods with high case numbers therefore impede economic recovery.
- Lastly, exposure to high infection risk over long time periods does not respect people’s inherent right to protection of their lives and physical integrity from harm.
We conclude that the containment strategy, which aims at keeping case numbers low, is more beneficial than widespread community spread in terms of health, the economy and society. At the same time, it is important to strengthen the surveillance-response plan to reduce case numbers in case of a resurgence: to have the tools to detect and monitor new cases, effective contact tracing, isolation and quarantine, and the resources to continue to provide excellent healthcare to people who get infected.
The development of vaccines and better treatments is progressing rapidly, but it will take some time until their safety can be established and they become widely available. It is therefore important that we continuously seek to improve the ways in which we keep SARS-CoV-2 under control, with minimal negative consequences for the economy and the freedom of individuals. We further advocate to continue to communicate Switzerland’s containment strategy clearly and explicitly to the population, while acknowledging challenges and uncertainties.
1) Strategic goal and key objectives
The ultimate goal of any COVID-19 control strategy is to reach normalization, that is, a situation where SARS-CoV-2 is no longer a burden on health, economy, or society. It will not be possible to eradicate this virus, which is now being transmitted globally. Normalization will therefore need to be based on population immunity against SARS-CoV-2 and the availability of effective treatment options. People can develop immunity through vaccination, or potentially through infection and recovery. The containment strategy aims at containing the spread of SARS-CoV-2 until immunity can be acquired through a safe and effective vaccine.
Some people have proposed that immunity in the population could be achieved through infection. Here, we evaluate the feasibility of this proposal, which we refer to as the “community infection approach” (“Durchseuchung” in German). In English, the phrase “achieving natural herd immunity” has been used. We do not use this term since it is, as we will discuss below, unclear whether infection with SARS-CoV-2 leads to long-lasting immunity.
When evaluating and comparing alternatives, one has to judge their consequences on public health, the economy and society both short and long-term. In general terms, overall quality of life should be preserved, with the following key objectives:
- Protect lives, the physical and mental health of the population, and all other fundamental human rights.
- Minimize the burden on the economy.
- Minimize the burden on society of the measures taken in terms of social isolation, impoverishment, discrimination, or loss of social cohesion.
2) The concept of the “community infection approach”
The basic idea of the “community infection approach” is that one would accept – or actively promote – widespread transmission of SARS-CoV-2 in the community. The number of people who are infected, or have been infected, would then increase over time. If infection leads to immunity (but see below), then the fraction of immune people in the population would increase over time and the fraction of susceptible people would decrease, so that the national epidemic would eventually slow down and reach a very low incidence or even come to a halt. Before discussing details, it is important to note that the fraction of people in Switzerland who have been infected until now is far below such a threshold. The observed seroprevalence (i.e. the fraction of people for which an antibody test indicates a past infection with SARS-CoV-2 ) is 1.6% in Zurich [1], 7% in Vaud [2], 8.9% in Ticino [3] and 10.8% in Geneva [4].
Different versions of the “community infection approach” have been proposed. It is of central importance to prevent the collapse of the healthcare system. In order to do that, the number of newly infected people per day would have to be kept constant at a level that does not exceed the capacity of the healthcare system. One version aims at reducing disease burden through protecting people who have a high risk of mortality or severe disease from infection.
All the approaches that seek to prevent the collapse of the healthcare system require state intervention. The only approach that would not require state intervention is to not try to control the epidemic at all. This would lead to the collapse of the healthcare system and would therefore violate the key objectives identified above.
3) Problems of the “community infection approach”
Here, we show why the “community infection approach” has fundamental flaws and would cause widespread damage to health, the economy and society.
It is not clear whether infection leads to lasting immunity. More specifically, it is not clear to what degree people who have been infected by SARS-CoV-2 are immune to future SARS-CoV-2 infections, and how long this immunity would last. In general, immunity induced by SARS-CoV-2 might be relatively weak and short-term. Weak or short-term immunity after infection would mean that the epidemic would not come to a halt once a large fraction of the population has been infected; rather, people could get infected and re-infected continuously. This aspect of immunity does not mean that one cannot develop a vaccine against SARS-CoV-2; vaccines can be designed to induce stronger and longer-lasting immune responses than those generated by an infection.
A “community infection approach” would have a massive health toll, in terms of mortality, severe disease and persistent health problems. Estimates of the infection fatality ratio for SARS-CoV-2 in Switzerland range between 0.5% and 1.0% (see Section 5.1 and [5]; this is an overall estimate, assuming that all age classes are infected at roughly equal proportions). This estimate assumes a functioning healthcare system; improved clinical care can increase survival, but so far, the improvements have been moderate. The shift, since May 2020, in the age profile of diagnosed infections towards younger age groups, has resulted in fewer hospitalisations and deaths, despite increasing numbers of new cases. This epidemiological pattern may give the impression that continued high levels of infection are tolerable. But increasing case numbers increase the risk that the infection will spread to older and more vulnerable population groups and mortality will increase again. If several million people in Switzerland were to be infected, the expected number of deaths would be in the tens of thousands even without the collapse of the healthcare system. This makes this approach incompatible with binding constitutional and international frameworks requiring that all reasonable measures are taken to prevent the loss of life and physical harm. These frameworks are not suspended during a pandemic.
In addition to the death toll, SARS-CoV-2 causes severe disease in a fraction of the patients. And among the patients with milder acute disease, between 10% and 30% experience persistent symptoms more than a month after the initial diagnosis ([6]and [7]). The type and frequency of deleterious long-term health effects is currently not well understood, and exposing the population at large to infection would represent a major risk.
It has been proposed that the health toll could be reduced by protecting the parts of the population at high risk of death or severe disease (for example, the elderly). However, features of this virus, and experience with this pandemic, show that such protection is likely to be impossible. SARS-CoV-2 is often transmitted before people have symptoms and are awae that they are infected. If case numbers are high – as any “community infection approach” would require – then it will not be possible to prevent presymptomatic carriers from infecting members of the risk groups. Isolating the vulnerable population is not feasible in practice and is socially undesirable. It is not realistic that people above a certain age or with certain health conditions are permanently separated from the rest of the population (for some, this would mean isolation for the rest of their lives) – they live in families, need health and other services. Also, any attempt to protect risk groups would need to be kept up over very long periods of time, as we will discuss.
Infecting a large population without collapse of the healthcare system takes a very long time. To prevent a collapse of the healthcare system, the “community infection approach” would need to achieve a high, but constant, level of transmission with – as an example, based on the following [8] – 10,000 new SARS-CoV-2 infections, 200 (~2% of infections) hospitalizations, 50 (~25% of hospitalizations) admissions to intensive care units, and 50 to 100 (0.5%-1.0% of infections) deaths in Switzerland per day. Assuming that patients stay in an intensive care unit (ICU) for 3 weeks on average, this level of transmission would correspond, on any given day, to around 1000 patients in intensive care on average (50 patients per day, of which each would stay on average for 21 days, corresponding to 50*21=1050 patients in intensive care). This is close to the current ICU capacity in Switzerland. Such a strategy would take about 430 days until half the population were infected. Even if infection led to long-lasting immunity (but see above), then an attempt to reach immunity through widespread community transmission would take in the range of 1-2 years. Since it is not clear whether infection induces robust and lasting immunity, any strategy that aims at widespread transmission in the community could lead to a long-lasting and severe epidemic in Switzerland.
A long period with high case numbers would cause massive damage to the economy and to society. Any “community infection approach” would attempt to keep the daily numbers of new infections at a high level (otherwise it would take even longer than 1-2 years to infect even half of the population). As we discuss in section 5.4 below, maintaining high case numbers prevents economic recovery. When case numbers are high, it is much more difficult to interrupt individual transmission events in a targeted way through a surveillance-response approach, and one would need to re-impose costly general measures. In addition, a rampant epidemic reduces people’s trust, increases uncertainty and decreases spending and investment.
High case numbers can also lead to direct costs to producing industry sectors if a substantial fraction of workers in a given company is ill or in quarantine at the same time, and can lead to a disruption of the public sector (such as education, healthcare and other public services).
As mentioned, strict general measures are needed to keep a situation with high case numbers under control, and these strict general measures impose costs on the economy and place restrictions on society and reduce the freedom of individuals. The point about economic costs is exemplified when comparing Switzerland with the US, the UK and Sweden: after Switzerland brought case numbers down in April 2020, it was able to abolish many of the general measures and overall recorded fewer fatalities relative to its population. While the US and Sweden experienced a similar decline in GDP as Switzerland, it was far more devastating in the UK. In addition, especially the UK and the US have had to maintain strict general measures for much longer (see [9]), which are damaging to the economy and society. The economic recovery of all three will probably take longer than in the case of Switzerland. For details see section 5.4. below.
A situation with high case numbers over extended periods of time also leads to a high burden in terms of limitations of fundamental rights (freedom of movement and travel, freedom of association and assembly, economic freedoms, political rights and participation, etc.). In additino, deliberately exposing people to a disease for which there is currently no cure does not respect their need to be protected from harm. Accepting high case numbers implies accepting high fatalities and severe health risks, which means the right to life and physical integrity (Swiss Federal Constitution Art. 10 §§ 1and 2, European Convention of Human Rights, Art. 2) are at stake. While this right cannot be protected absolutely, state authorities as a rule are under an obligation to make their best efforts to protect it.
4) Conclusions
Our analysis shows that pursuing a “community infection approach” would lead to massive damage to health, the economy and society. Maintaining low case numbers is therefore beneficial for everyone: it protects us from disease, prevents any further regional and national lockdowns and thereby allows economic recovery, and provides society with an outlook for more freedom and better well-being.
The effectiveness of any strategy hinges on the participation of the population. In line with a previous policy brief [10], we emphasize that participation and communication with all parts of the population are key. Thus, we propose that Switzerland’s strategy is more explicitly communicated to and with the population. The federal and cantonal authorities should develop a clear and transparent narrative that gives an honest vision for the future, while acknowledging the challenges and uncertainties. This vision should include efforts to find and implement measures to minimize infringements on fundamental rights, obligations, and freedoms.
At the same time, we should prepare for times when case numbers increase. Switzerland must have the tools to monitor the epidemiological situation accurately and in real-time; resources and personnel to continue to provide excellent healthcare and respond to the social and economic needs of people who get infected; and a clear surveillance-response plan to react quickly and bring case numbers down again.
We emphasize that the goal of the containment strategy is to solve the COVID-19 crisis through vaccination and improved medical treatment, and that Switzerland should make every conceivable effort to support and be involved in the development and equitable distribution of vaccines and treatments.
The road ahead to resolve the COVID-19 crisis will not be easy. It is likely that vaccines and better treatments will be developed within the next year, but it will take a while until their safety can be established and until they are widely available. It is therefore important that we continuously seek to improve the ways to keep SARS-CoV-2 under control with minimal negative impacts on the economy and the freedom of individuals.
5. Appendix: Current evidence and important parameters
5.1. Mortality and health effects of COVID-19
Mortality risk of COVID-19
The overall proportion of deaths among all SARS-CoV-2 infections (infection fatality ratio, IFR) for the general population in Switzerland has been consistently estimated around 0.5%-1.0% (Table 1; these estimates are from the first phase of the pandemic). These estimates are also consistent with the assessment of the World Health Organization (WHO) (source). The estimated IFR is corrected for the fact that a large proportion of the SARS-CoV-2 are not detected because they are mildly symptomatic or even asymptomatic. This is an overall estimate, assuming that all age classes are infected at roughly equal proportions.
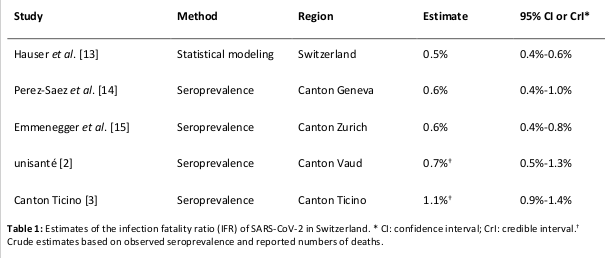
A second and different proxy of mortality is the case fatality ratio CFR, the proportion of deaths among identified confirmed cases. Due to underascertainment of SARS-CoV-2 infections, the CFR is typically higher than the IFR. After March/April 2020, the CFR in Switzerland decreased, when the numbers of hospital admissions, ICU admissions and deaths decreased and the number of documented SARS-CoV-2 infections increased. Several factors likely contributed to this decrease. The probably dominant factor was an increase in testing and an increased fraction of transmission in people of younger age with fewer risk factors. Improved therapies might also play a role, even though the evidence of decreased mortality by any therapy is limited to the corticosteroid dexamethasone for patients who are critically ill. There is no evidence that this decrease of CRF in Switzerland is due to changes in the properties of the virus; genetic changes in SARS-CoV-2 are continuously monitored and potential effects on the severity of infection evaluated [11]; in Switzerland, there was no major shift in the SARS-CoV-2 strains that would be indicative of a selective sweep of a strain with altered properties [12].
Long-term health effects of COVID-19
Even if long-term consequences of SARS-CoV-2 infection are highly probable, long-term observations are not yet available because of the short time since the beginning of the pandemic. The following publications provide an overview of the current considerations [16, 17]. There are different categories of long-term consequences:
- Patients who are critically ill with severe COVID-19 and survive their ICU stay, with a high risk of post-ICU syndrome, similar to what is seen for severe sepsis or patients with acute respiratory distress syndrome.
- Patients with chronic diseases that are exacerbated or aggravated by SARS-CoV-2 infection.
- Frail elderly patients who experience a decrease in muscle tone or endurance after the infection.
- Patients with neurological, cardiovascular, digestive or respiratory conditions that are a consequence of SARS-CoV-2 infection.
- Patients with more general and persistent non-specific symptoms, such as chronic fatigue [18].
For the last two categories, it is difficult, at this stage, to differentiate association from a direct causal effect of the viral infection. Nevertheless, it is probable that many patients may have long-term consequences and a decreased quality of life in the months following the pandemic.
5.2. Immunity to SARS-CoV-2
This topic will be discussed in more depth in an upcoming policy brief by the task force. Here we only provide a short summary.
Immunity after SARS-CoV-2 infection
On average, immunity induced by SARS-CoV-2 might be relatively weak and short-term. The majority of infected persons may lose immune protection as early as after a few weeks or months. Although it is too early to be sure about this, the available data suggest that immune responses to SARS-CoV-2 infection is not stronger than to the common cold Coronaviruses which also induce only weak and short-term immunity.
Cross-immunity
Unfortunately, there is no evidence that common cold Coronaviruses induce cross-immunity mediating neutralizing antibodies (nAbs). In contrast, these viruses induce some cross-specific non-neutralizing antibodies and some T cells. Such T cells may reduce COVID-19 severity (to be confirmed by dedicated studies). The same may be the case for the T cells induced by previous infection with SARS-CoV-2. However, reduction in the rates of infection and transmission is unlikely, because T cells in absence of nAbs can hardly prevent infection.
Levels of immunity required for herd immunity
(here we use the term herd immunity in a technical sense to refer to the fraction of individuals in a population that needs to be immune so that an infectious disease can no longer spread)
Natural infection is unlikely to induce herd immunity, because immunity is weak and short-term. Herd immunity means that the population (the “herd”) is immune and the virus can no longer circulate because of this broad degree of immunity. Herd immunity is usually achieved by successful vaccines but not by natural infection.
The herd immunity threshold is typically determined by 1-1/R0 , which corresponds to 60% for a basic reproduction number R0 of 2.5 [8, 19]. Some modeling studies suggest that herd immunity thresholds can be lower due to the heterogeneity in contact rates and individual susceptibility. However, these studies are typically based on the assumption of static contact networks that do not reflect the dynamics of real-world community structures. Furthermore, results from seroprevalence studies in areas with high infection attack rates support the standard estimate for the herd immunity threshold (42% in Ischgl, Austria [20]; 52% in Corona, Queens, New York City, US [21]; 62 % in Bergamo, Italy [22]). The observed seroprevalence in different cantons in Switzerland is considerably lower and far below the threshold: 1.6% in Zurich [1], 7% in Vaud [2], 8.9% in Ticino [3] and 10.8% in Geneva [4]).
It is again important to keep in mind that it is currently not known whether infection with SARS-CoV-2 leads to long-term immunity.
5.3. Prospects for the development of vaccines and effective treatment strategies
Prospects for the development of an effective vaccine
The worldwide COVID-19 vaccine development is broad, fast and powerful. Several phase 1+2 data show that some vaccines induce stronger immune responses than natural infection. Provided that phase 3 data readily demonstrate efficacy and safety, we expect that first vaccination will become available during the year 2021. Clinical studies may, however, show that more efforts are needed, which would mean further delays (as for example during the development of the AstraZeneca Oxford SARS-CoV-2 vaccine [23]) .
Prospects for the development of effective treatment strategies
In situations and countries where hospital mortality is high, repurposed antiviral drugs lead to a reduction of this mortality. However, Switzerland has shown one of the lowest hospital mortalities worldwide, and these drugs are therefore expected to be less effective in Switzerland.
Specifically developed drugs are entering the study arena, i.e. phase I-II trials. Among them are drugs inhibiting replication of the virus or drugs working as neutralizing antibodies. The timescale when drugs with highly significant effects can routinely be used is difficult to predict, but arrival before summer 2021 is unlikely.
5.4. Control measures determine the rate of change in case numbers but not their absolute value
One motivation for suggesting an “community infection approach” is the intuition that this might allow Switzerland to use less strict control measures and therefore ease the burden on the economy and the society. However, a careful analysis of the link between control measures and the dynamics of the infection indicates that this intuition is incorrect.
First, it is important to clarify how the measures one implements – for example, limiting the size of gatherings or closing certain venues – influence the development of the case numbers. One might intuitively think that the measures directly determine the number of new cases occurring per day: that strict measures lead to a constant low number of new cases and loose measures lead to a constant high number of new cases. However, and very importantly, this is not the case.
The measures taken determine how rapidly the number of cases grows, rather than the number of cases per se: they determine whether case numbers increase and how rapidly they increase. This means that easing measures does not lead to a higher constant number of cases; rather, if case numbers begin to increase, they will continue to increase. Since it is essential to prevent an uncontrolled increase in case numbers (to protect the healthcare system from collapsing), it is essential to maintain a combination of measures that, together with an effective surveillance-response strategy, reduces the growth rate of the number of cases to zero or below.
Second, it is important to clarify what the effort is – in terms of costs to the economy and to society – that is required to maintain case numbers at a certain level. One might intuitively think that it is less costly to maintain case numbers at intermediate levels (e.g., 500 new cases per day) than at low levels (e.g., 20 new cases per day). However, this intuition is also wrong, for two reasons. The first reason is that, as discussed above, the stringency of the measures taken determines the rate at which the epidemic grows, rather than the absolute case number. The same set of measures that is effective at maintaining case numbers at 500 new cases per day will also be effective at maintaining case numbers at 20 new cases per day. The second reason is that, once case numbers are low, one can replace costly measures with less expensive measures. At high case numbers, it is harder to disrupt individual chains of transmission, because too many people are infected. One therefore has to impose general measures that impact the whole population, not just those potentially infected. These measures tend to have high economic costs and are disruptive to society. At low case numbers, one can replace some of these general measures with highly targeted measures – interventions that focus on the people that are most likely infected, and therefore only affect a small fraction of the population. These targeted measures therefore have lower costs, both economically as well as in terms of the burden on society. This has important consequences: if one needs to control case numbers (as is central to strategies 1, 3 and 4), the costs to the economy and society are lower if the number of new cases per day is kept low.
To summarize, it is less costly and more beneficial for the economy and society to control the epidemic at low case numbers. This fact is important to keep in mind when comparing different possible approaches for controlling SARS-CoV-2.
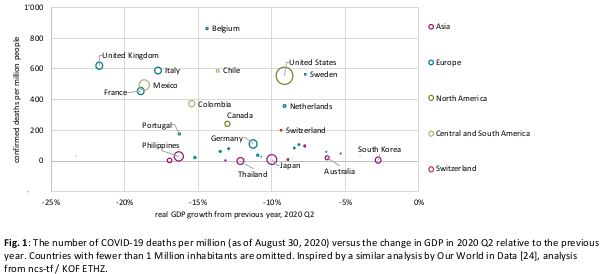
This conclusion is also supported by analyzing the relationship between the economic impact and the health impacts of COVID-19 in different countries (Fig. 1). Countries with the highest COVID-19 death rate also tend to have suffered the most severe economic downturns. While such associations do not establish causation, the pattern is consistent with the perspective that high case numbers require that general measures are imposed, which tend to be more costly and disruptive for the economy.
- Emmenegger M, De Cecco E, Lamparter D, Jacquat RPB, Ebner D, Schneider MM, et al. Early peak and rapid decline of SARS-CoV-2 seroprevalence in a Swiss metropolitan region. medRxiv. 2020:2020.05.31.20118554. doi: 10.1101/2020.05.31.20118554.
- unisanté. COVID-19: 7% des vaudois·es infecté·e·s 2020 [updated 08.06.2020]. Available from: https://www.unisante.ch/fr/unisante/actualites/covid-19-7-vaudoises-infectees.
- Repubblica e Cantone Ticino Ddseds. Coronavirus: risultati dello studio di sieroprevalenza del virus SARS-CoV-2 nella
popolazione ticinese 06.07.2020. Available from: https://www4.ti.ch/area-media/comunicati/dettaglio-comunicato/?NEWS_ID=188153&tx_tichareamedia_comunicazioni%5Baction%5D=show&tx_tichareamedia_comunicazioni%5Bc ontroller%5D=Comunicazioni&cHash=bea1ca89d443e685b2a9079f42186b3d.
Stringhini S, Wisniak A, Piumatti G, Azman AS, Lauer SA, Baysson H, et al. Seroprevalence of anti-SARS-CoV-2 IgG antibodies in Geneva, Switzerland (SEROCoV-POP): a population-based study. The Lancet. 2020;396(10247):313-9. doi: 10.1016/S0140-6736(20)31304-0.
ncs-tf. Risk factors for severe manifestations of SARS-CoV-2 infection. 2020. Available from: https://ncs-tf.ch/de/policy-briefs/risk-factors-for-severe-manifestations-of-sars-cov-2-infection-27-july-20-en-2/download
Tenforde MW, Kim SS, Lindsell CJ, Rose EB, Shapiro NI, Files DC, et al. Symptom duration and risk factors for delayed return to usual health among outpatients with COVID-19 in a multistate health care systems network—United States, March–June 2020. Morbidity and Mortality Weekly Report. 2020;69(30):993.
Greenhalgh T, Knight M, Buxton M, Husain L. Management of post-acute covid-19 in primary care. bmj. 2020;370.
Lemaitre JC, Perez-Saez J, Azman A, Rinaldo A, Fellay J. Assessing the impact of non-pharmaceutical interventions on SARS-CoV-2 transmission in Switzerland. medRxiv. 2020.
Hale T, Webster S, Petherick A, Phillips T, Beatriz K. COVID-19: Government Response Stringency Index. 2020.
ncs-tf. Communication and SARS-CoV-2 2020. Available from: https://ncs-tf.ch/de/policy-briefs/communication-and-sars-cov-2-30-july-en-2/download.
Young BE, Fong S-W, Chan Y-H, Mak T-M, Ang LW, Anderson DE, et al. Effects of a major deletion in the SARS-CoV-2 genome on the severity of infection and the inflammatory response: an observational cohort study. The Lancet. 2020.
Hodcroft E, Neher R, Nadeau S, Stadler T. Phylogenetic analysis of Swiss SARS-CoV-2 genomes in their international context [cited 2020]. Available from: https://nextstrain.org/groups/swiss/ncov/switzerland.
Hauser A, Counotte MJ, Margossian CC, Konstantinoudis G, Low N, Althaus CL, et al. Estimation of SARS-CoV-2 mortality during the early stages of an epidemic: A modeling study in Hubei, China, and six regions in Europe. PLOS Medicine. 2020;17(7):e1003189. doi: 10.1371/journal.pmed.1003189.
Perez-Saez J, Lauer SA, Kaiser L, Regard S, Delaporte E, Guessous I, et al. Serology-informed estimates of SARS-COV-2 infection fatality risk in Geneva, Switzerland. medRxiv. 2020.
Emmenegger M, De Cecco E, Lamparter D, Jacquat RP, Ebner D, Schneider MM, et al. Early peak and rapid decline of SARS-CoV-2 seroprevalence in a Swiss metropolitan region. medRxiv. 2020.
Yelin D, Wirtheim E, Vetter P, Kalil AC, Bruchfeld J, Runold M, et al. Long-term consequences of COVID-19: research needs. The Lancet Infectious Diseases. 2020.
Palmer K, Monaco A, Kivipelto M, Onder G, Maggi S, Michel J-P, et al. The potential long-term impact of the COVID-19 outbreak on patients with non-communicable diseases in Europe: consequences for healthy ageing. Aging Clinical and Experimental Research. 2020:1.
Rimmer A. Covid-19: Impact of long term symptoms will be profound, warns BMA. BMJ. 2020;370:m3218. doi: 10.1136/bmj.m3218.
Althaus CL, Probst D, Hauser A, Riou JL. Time is of the essence: containment of the SARS-CoV-2 epidemic in Switzerland from February to May 2020. medRxiv. 2020.
Knabl L, Mitra T, Kimpel J, Roessler A, Volland A, Walser A, et al. High SARS-CoV-2 Seroprevalence in Children and Adults in the Austrian Ski Resort Ischgl. medRxiv. 2020.
Goldstein J. 1.5 Million Antibody Tests Show What Parts of N.Y.C. Were Hit Hardest 2020. Available from: https://www.nytimes.com/2020/08/19/nyregion/new-york-city-antibody-test.html.
Regione Lombardia SSS. Coronavirus: in Bergamasca 3.320 test sierologici tra operatori sanitari e cittadinanza 2020. Available from: http://www.ats-bg.it/upload/asl_bergamo/gestionedocumentale/CSATSBG2020-04-30CSATSBG2020-04-30coronavirusesitisierologici_784_31010.pdf.
Phillips N, Cyranoski D, Mallapaty S. A leading coronavirus vaccine trial is on hold: scientists react. Nature. 2020. Epub 2020/09/11. doi: 10.1038/d41586-020-02594-w. PubMed PMID: 32908295.
Hasell J. Which countries have protected both health and the economy in the pandemic? 2020. Available from: https://ourworldindata.org/covid-health-economy.
Date of request: –
Date of response: 14/9/2020
In response to request from: –
Comment on planned updates: –
Expert groups and individuals involved: –
Contact persons: Martin Ackermann, Manuel Battegay, Samia Hurst, Monika Buetler, Marcel Tanner, Sebastian
Bonhoeffer