– Policy Brief
Questions
Are there identified risk factors for a) hospitalization, b) ICU admission, and c) mortality in the context of COVID-19 and SARS-CoV-2 infection?
Summary
The evaluation of the risk of hospital and ICU admission, as well as the mortality associated with the COVID-19 is an important tool to plan the necessary resources to manage and care for patients, and to evaluate the consequences of the disease. The high number of infected patients around the world has led to the publication of a large amount of data. For each specific question, this policy brief includes the highest level and most updated available evidence, and highlight remaining uncertainties.
Main text
Question 1. What are the identified risk factors for hospitalization in patients with SARS-CoV-2 infection?
Introductory note: Hospitalizations for COVID-19 can be grouped into 4 categories: 1) medical reasons as direct consequence of SARS-CoV-2; 2) medical/social reasons, but not directly associated to SARS-CoV-2 , e.g. elderly patient not able to care for him/herself; 3) patients or physician-related causes: fear of the disease, or potential for adverse outcome, but no clinical necessity, and 4) for reasons of isolation or cohorting patients, without clinical necessity.
This review will focus on group 1, which is largest group in Switzerland. The hospitalization rate of SARS-CoV-2 infection is highly variable around the worldm depending on the structure of the population and the organization of the healthcare system. A modelling study from France suggests that around 3.6% of infected individuals are hospitalized (95% CrI: 2.1–5.6) (Salje). Since March 2020, 7.3 % of confirmed infections lead to an hospital admission in Switzerland (FOPH) :

Many risk factors associated with hospital admission have been described (Salje – Guan – Richardson – Zhou – Petrelli):
- increasing age, with no specific limit (Salje – CDC – Lewnard – Petrelli)
- male gender (RR 1.25, 95% CrI: 1.22–1.29) (Salje)
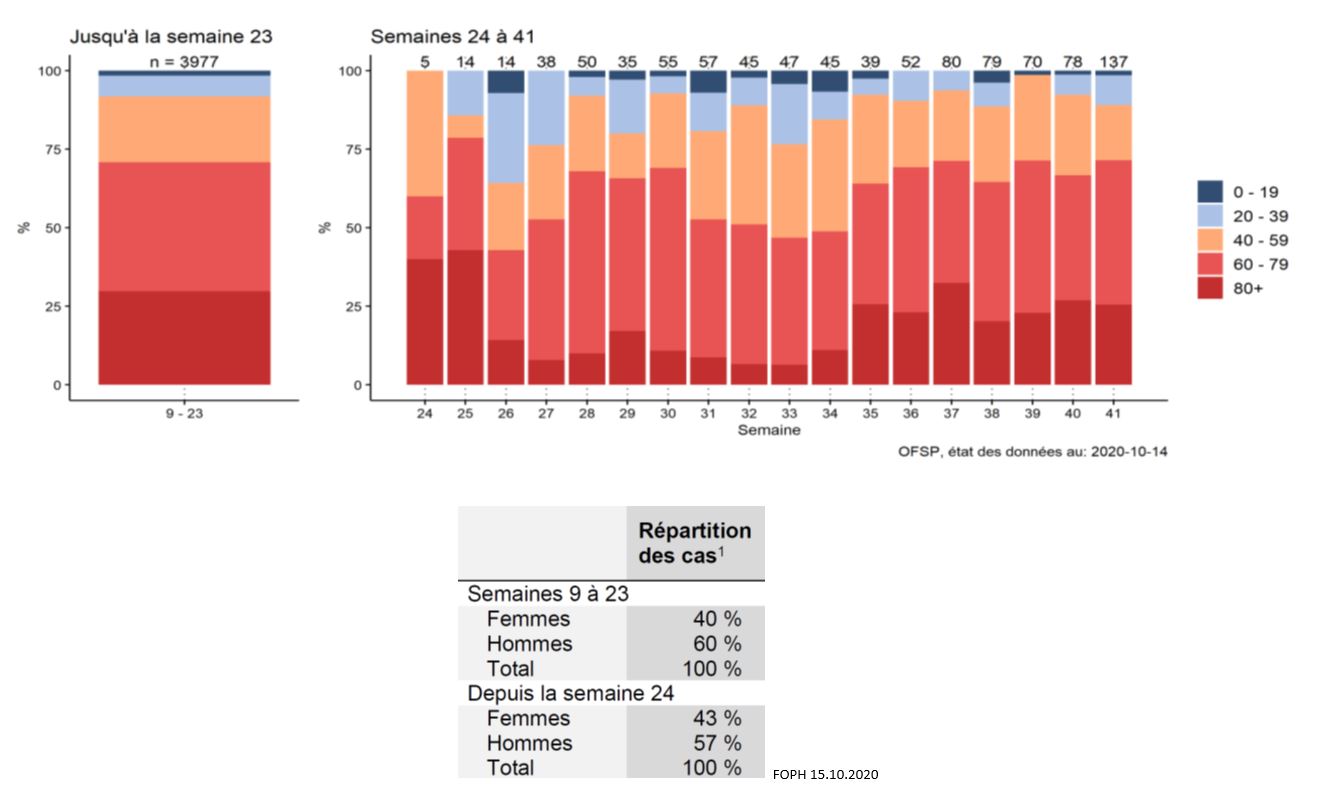
These data are concordant with the age and sex distribution of hospitalized patients in Switzerland (FOPH 15.10.2020) :
Comorbidities :
- hypertension and cardiovascular diseases (arrhythmia, heart failure, ischemic heart disease, chronic kidney disease) (Petrelli)
- obesity is associated with a 2.13 increased risk (Popkin)
- chronic respiratory disease, particularly COPD (RR 1.88, 95% CI, 1.4–2.4) (Alqahtani).
- diabetes
- smoking (RR 1.45, 95% CI: 1.03–2.04) (Alqahtani).
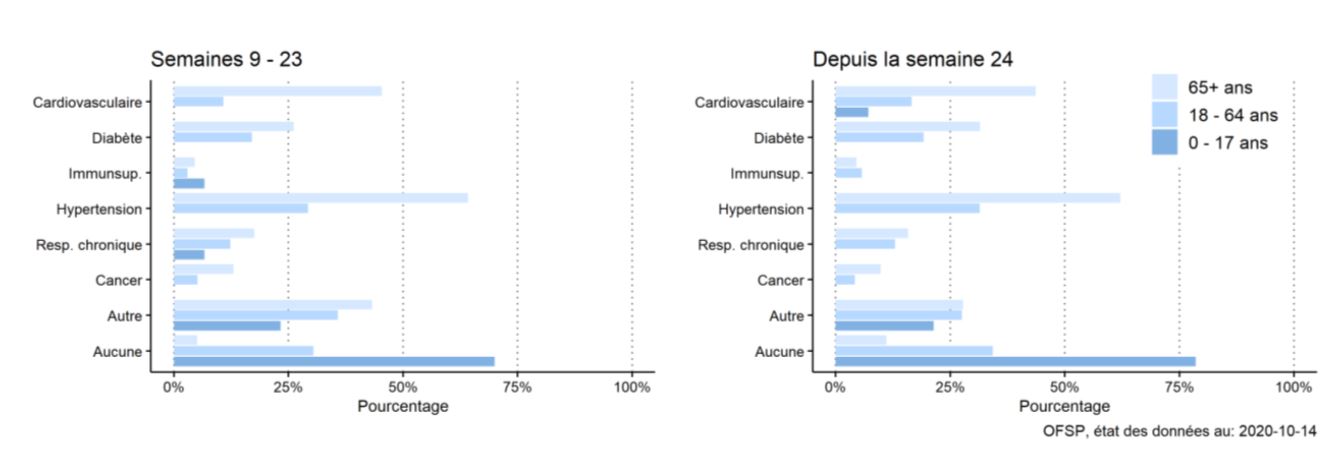
These risk factors are intertwined and sometimes merely associated with age. But, comorbidities are present in over 80 % of hospitalized patients in Switzerland, which is concordant with the published literature (Salive) :
Some prognosis model have been published, but without external validation, limiting their use (Wynants).
An on-line calculator is available (https://riskcalc.org/COVID19Hospitalization/), but has not been validated for Swiss patients (Jehli)
Uncertainty: The risk of an adverse outcome and hospitalization increases with age, male sex, obesity, and with the number of cardiovascular and pulmonary co-morbidities. The risk increase is gradual and additional factors such as host response, inoculum, genetic factors, and others may play a role on the individual level. No validated evaluation tool is available for the Swiss population to identify patients at high risk who may benefit from a preemptive of prophylactic therapy.
Question 2. What are the identified risk factors for ICU admission or development of severe disease in patients with SARS-CoV-2 infection?
Introductory note: ICU admission is indicated for patients needing continuous monitoring or complex therapies, such as mechanical ventilation and other organ support, that are not available on regular wards. The proportion of patients who need to be admitted to the ICU has been reported to be between 5 to 25 % (Guan 2 – Grasselli – Salje). A recent meta-analysis reported a total of 17% of hospitalized patients requiring intensive care (33 studies, 7504 patients), 9% invasive ventilation (45 studies, 6933 patients) and 2% extra-corporeal membrane oxygenation (12 studies, 1,486 patients) (Grant).
Many factors associated with ICU admission are not risk factors but rather parameters determining the indication for ICU admission.
Epidemiologic factors associated with ICU admission:
- age is associated with the development of a severe disease needing ICU admission (MMWR – Grasselli – CDC – Lewnard), as an independent risk factor (OR, 1.03; 95% CI, 1.01-1.05) (Liang). A French modelling study confirmed this, but with a decrease of risk over 70 (Salje)
- male sex is associated with ICU admission risk (RR: 1.61, 95% CI: 1.56–1.67) (Salje), although not uniformly reported (Guan 2 – Grasselli – CDC)
- co-morbid conditions (chronic heart or lung disease, hypertension, diabetes) are present in 70-80 % patients (Grasselli – Jain). Globally, the number of comorbidities is an independent predictive factor for the development of severe disease (OR, 1.60; 95% CI, 1.27-2.00) (Liang)
- COPD seems to be associated with a significant risk (OR 17.8, 95 % Ci 6.56-48.2) (Jain)
- obesity is associated with a 1.74 higher risk of ICU admission (Popkin)
- cardiovascular disease and hypertension are associated with an increased risk of ICU admission of 4.4 and 3.7 times respectively (Jain).
- diabetes is associated with ICU admission and short term outcome (Roncon)
- cancer history is an independent predictor of the development of a severe infection (OR, 4.07; 95% CI, 1.23-13.43) (Liang)
- transplanted patients may have an increased risk, but this is not definitely proven
- Smoking is associated with more severe disease, and possibly with increased risk of ICU admission (Alqahtani)
Clinical presentation associated with ICU admission:
- acute hypoxemic respiratory failure (rarely with hypercapnia)
- dyspnea is an independent predictive factor for a severe disease, with an OR between 2 to 6 (Liang – Jain)
- hemoptysis is an independent predictive factor for a severe disease (OR, 4.53; 95% CI, 1.36-15.15) (Liang).
- alterations in consciousness are associated with severe disease (OR, 4.71; 95% CI, 1.39-15.98) (Liang)
Laboratory findings associated with ICU admission :
- various laboratory parameters have been associated with ICU admission, mostly in observational series and univariate analysis, with high risk of bias.
- a large Chinese observational study identified several independent predictors (Liang) :
- neutrophil-to-lymphocyte ratio (OR, 1.06; 95% CI, 1.02-1.10)
- lactate dehydrogenase (OR,1.002; 95% CI, 1.001-1.004)
- direct bilirubin (OR, 1.15; 95% CI, 1.06-1.24)
- a meta-analysis and meta-regression identified the following factors (Zhang JJY) :
- raised leukocyte count (p<0.0001)
- raised alanine aminotransferase (p=0.024) and aspartate transaminase (p=0.0040)
- elevated lactate dehydrogenase (LDH) (p<0.0001)
- increased procalcitonin (p<0.0001)
Chest imaging pattern associated with ICU admission:
- any chest radiographic abnormality is associated with the development of a severe disease (OR, 3.39; 95% CI, 2.14-5.38) (Liang)
- patients with an acute respiratory failure frequently have an ARDS pattern on CT-scan and lung ultrasound, but with no specific diagnostic or prognostic value
Predicting tools and nomograms:
- many tools were developed on small and selected populations (Gong – Liang), with poor overall quality and no prospective external validation, and therefore limited usefulness (Wynants)
- The PREDI-CO model has fair operative characteristics (sensitivity 80% (73%–85%), specificity 76% (70%–81%), positive predictive 69% (60%–74%) and negative predictive 85% (80%–89), even though it has not been validated for the Swiss population (Bartoletti).
Uncertainty: ICU admission criteria may greatly vary between countries and institutions, depending on the number of available beds, the existence of intermediate care or step-down units, and the level of care, and this may influence the ICU admission rate. Published data show that age, male sex, and comorbid conditions are significant risk factors, and acute respiratory failure at admission and/or ARDS pattern on chest imaging are associated with ICU admission. The use of predictive model is still not recommended for individual risk prediction for patients in Switzerland.
Question 3. What are the identified risk factors for mortality in patients with SARS-CoV-2 infection?
Introductory note: General mortality (case fatality) is estimated between 0.7 and 3.6 % (CEBM – Williamson – Verity), and the Infection Fatality Ratio (IFR) that was estimated around 0.65-0.70% (Salje – Verity) is probably lower, around 0.27 according to the WHO (Ioannidis). In Switzerland, the mortality of confirmed cases is 2.4 % at this stage. The mortality rate of hospitalized patients was initially estimated around 18.1% (95% CI: 17.8–18.4) (Salje), but is probably closer to 7%, according to a recent meta-analysis (Grant). ICU mortality varies very much and is reported to be 37 % in the US (Gupta) and 45 % in Lombardy (Grasselli 2), and around 24% in a recent registry including Swiss patients (Wendel-Garcia). The mortality in nursing home resident is probably around 35%.
Positive results of clinical trial could modify the therapy and influence the mortality rate and the associated risk.
Many factors associated with a higher mortality have been identified :
Factors associated with mortality in the general population (CDC 2020):
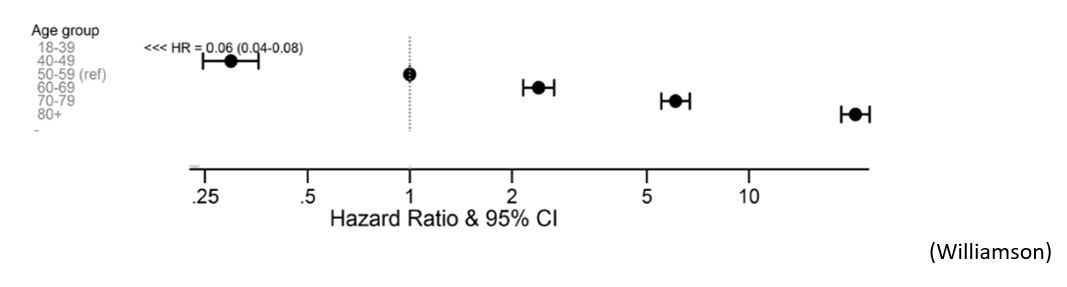
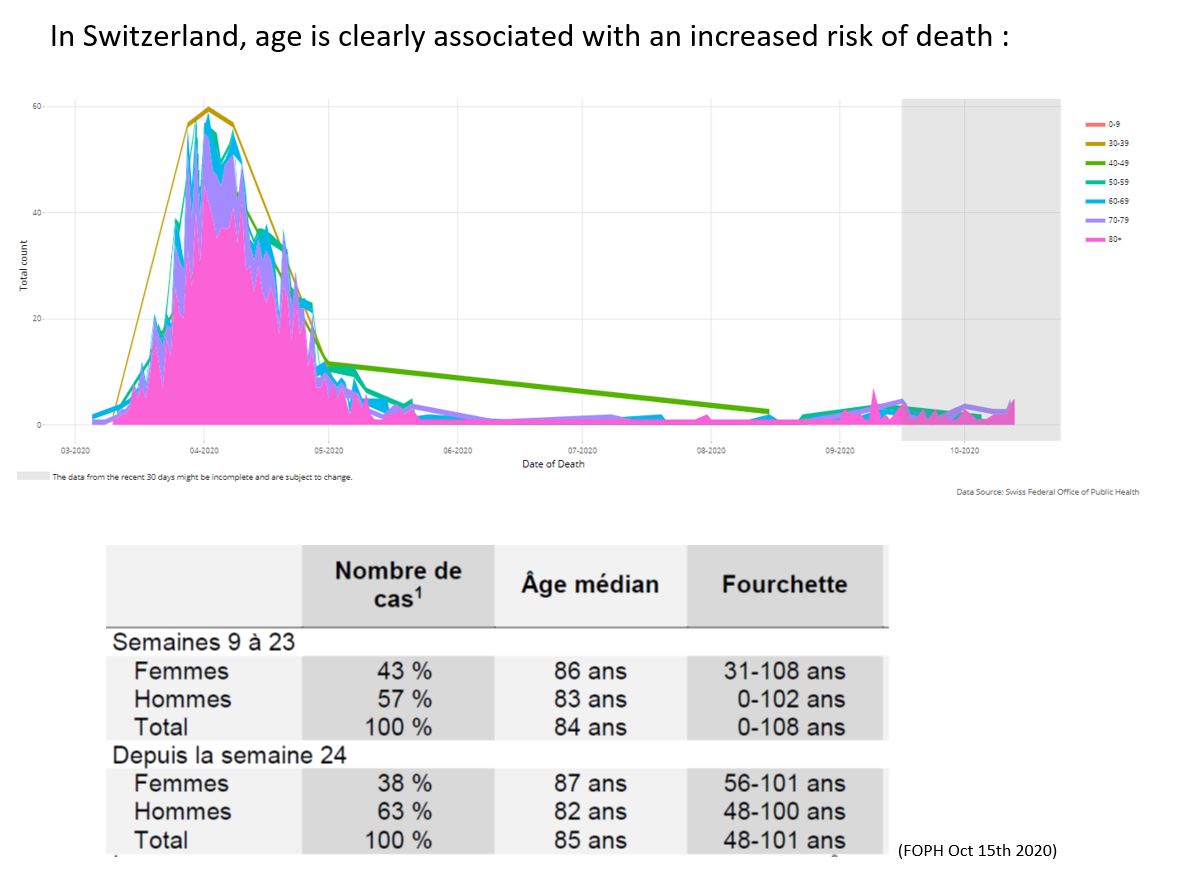
- Age is clearly associated with an increased risk the risk of dying (Knight – Lewnard – Petrelli – Williamson), from 0.001% under 20 to 10.1% over 80 (Salje).
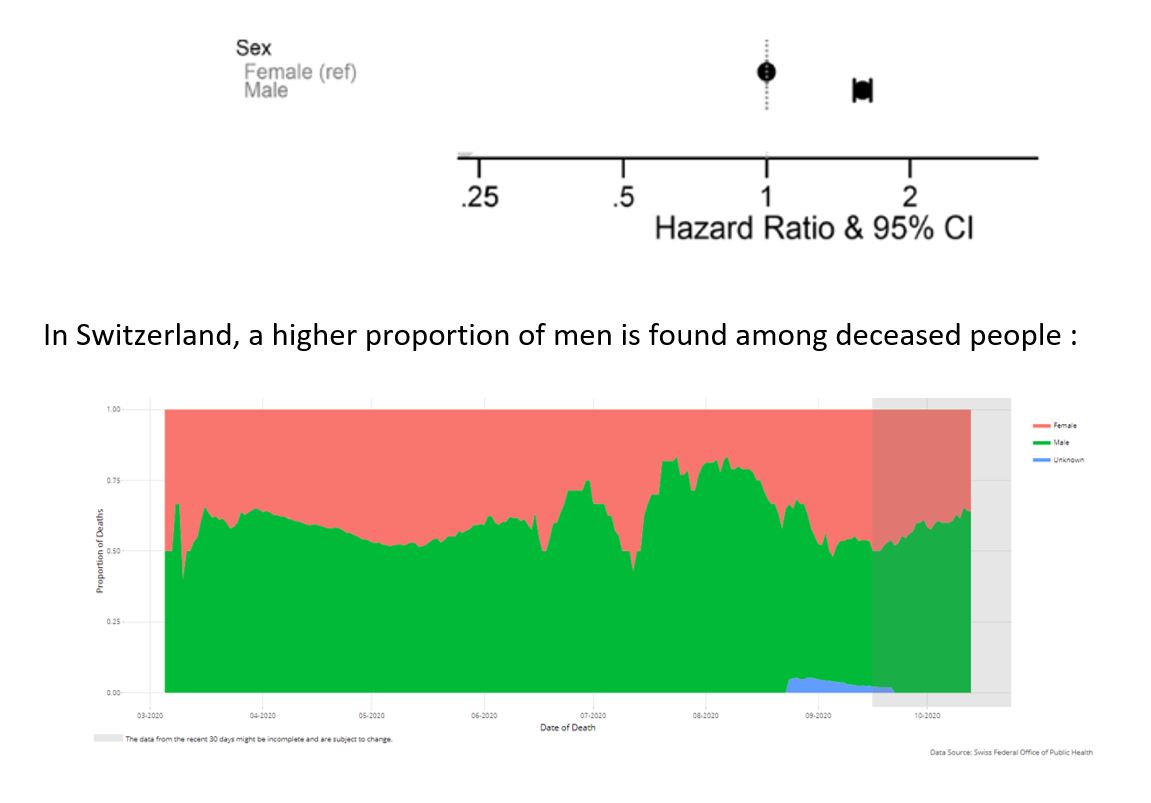
- male sex (Salje – Williamson) :
- Other factors associated with mortality :
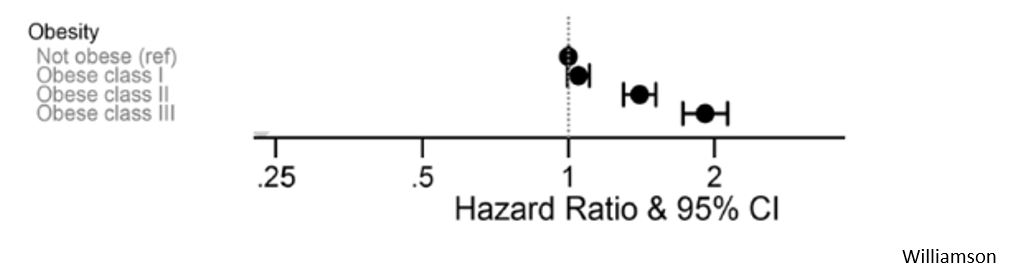
- obesity is associated with a 48 % increased risk of dying (Popkin -Williamson)
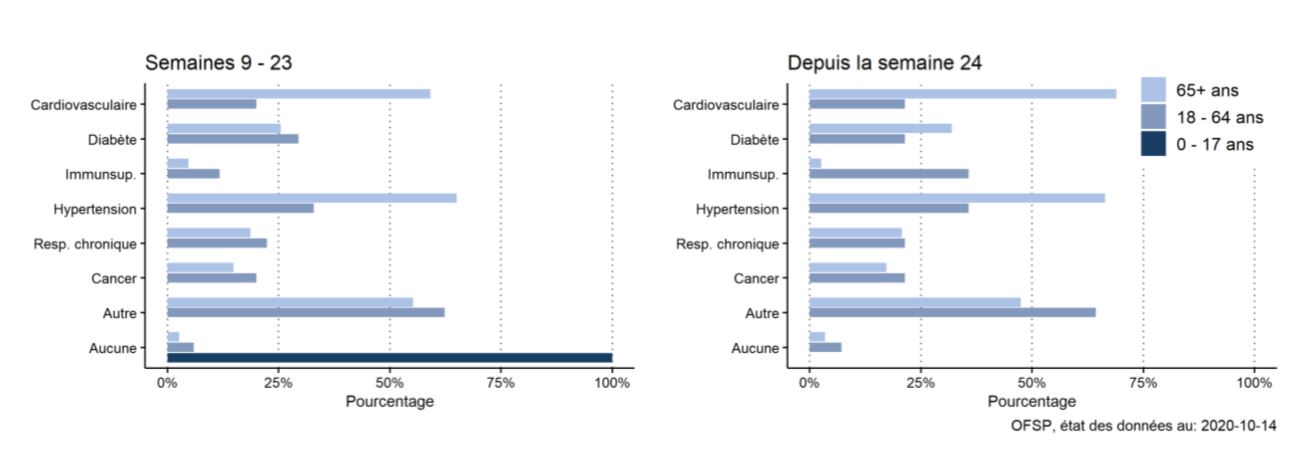
- comorbid conditions (CDC – Williamson), particularly :
- heart failure (Petrelli)
- dementia
- chronic liver disease
- diabetes (Petrelli – Williamson)
- nursing home residency (CDC)
- chronic immunosuppression (Williamson)
- cancer (Petrelli – Williamson)
- comorbid conditions (CDC – Williamson), particularly :
In Switzerland, the majority of deceased patient had at least one comorbitidy, in accordance with these data :
Factors NOT associated with mortality in the population (Reynolds):
- antihypertensive treatment, including ACE inhibitors and angiotensin-receptor blockers (Mackey)
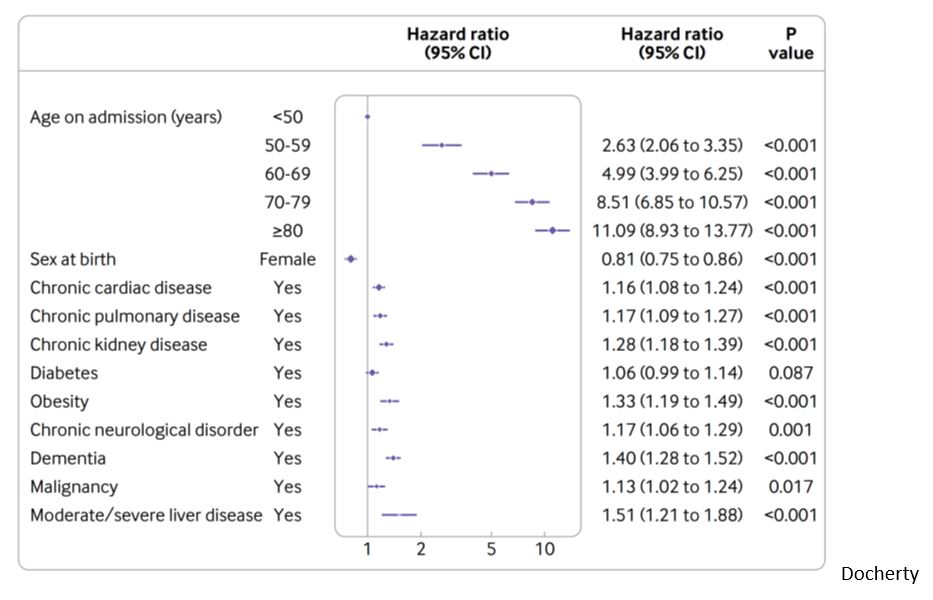
Independent factors associated with mortality in hospitalized patients (Liu – Ruan – Docherty):
- increasing age, starting from 50 year old
- sex: female sex is associated with decrease mortality : HR 0.81 (CI 0.75 to 0.86) (Docherty – Knight)
- coronary artery disease : OR 2.70 (95% CI 2.08 – 3.51)
- heart failure : OR 2.48 (95% CI 1.62 – 3.79)
- cardiac arrhythmia : OR 1.95 (95% CI 1.33 – 2.86)
- COPD : OR 2.96 (95% CI 2.00 – 4.40)
- current smoking : OR 1.79 (95% CI 1.29 to 2.47)
- smoking and COPD have also been associated with increased mortality in a meta-analysis (Alqahtani)
- obesity (Docherty)
Factor NOT associated with mortality in hospitalized patients (Mancia – Reynolds – Zhang P):
- antihypertensive treatment, including ACE inhibitors and angiotensin-receptor blockers
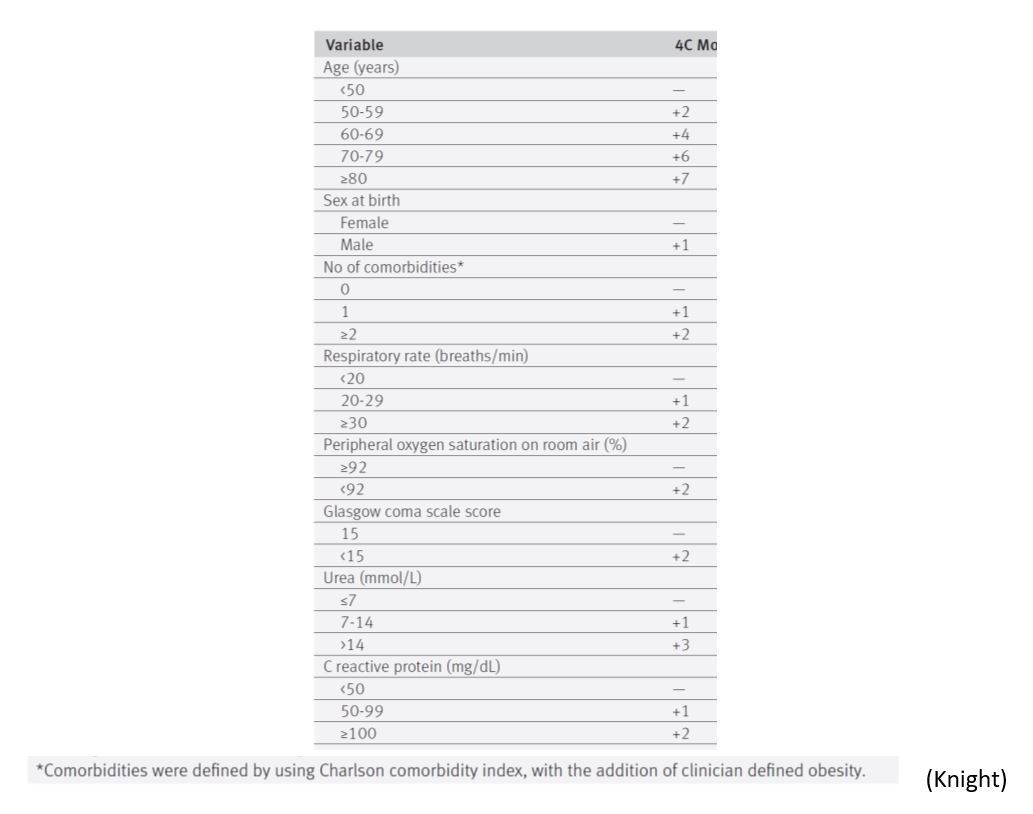
The 4C Mortality Score proposed by the WHO, based on the ISARIC cohort, is a risk stratification model for the prediction of death in hospitalized patients (Knight). It categorises patients in low, intermediate, high, or very high risk of death, based on easy-to-obtain parameters, but it has not been validated for Swiss patients:
Factors associated with mortality in the ICU:
- age is associated with ICU mortality (CDC – Qian – Grasselli 2 – Gupta), as an independent factor, with an hazard ratio of 1.75 (95% CI, 1.60-1.92) (Grasselli 2), and an OR of 11.15 (95%CI, 6.19-20.06) for over 80 years vs less than 40 (Gupta).

- acute respiratory distress syndrome (ARDS) and sepsis reported in 100 % of dying ICU COVID-19 patients (Chen)
- male sex (HR1.57; 95%CI, 1.31-1.88), high oxygen (HR, 1.14; 95%CI, 1.10-1.19) and PEEP (HR, 1.04; 95%CI, 1.01-1.06) need, low PaO2:FiO2 ratio (HR, 0.80; 95%CI, 0.74-0.87) on ICU admission are independently associated with ICU mortality (Grasselli 2 – Gupta)
- history of chronic obstructive pulmonary disease (HR, 1.68; 95%CI, 1.28-2.19), hypercholesterolemia (HR, 1.25; 95%CI, 1.02-1.52), and type 2 diabetes (HR, 1.18; 95%CI, 1.01-1.39), higher body mass index (>40 vs <25: OR, 1.51; 95%CI, 1.01-2.25), and active cancer (OR, 2.15; 95%CI, 1.35-3.43) are also independently associated with higher mortality (Grasselli 2 – Gupta)
- no validated prediction models has been validated, as they were derived from small cohorts of selected patients, with a high risk of bias, no or poor external validation (Wynants)
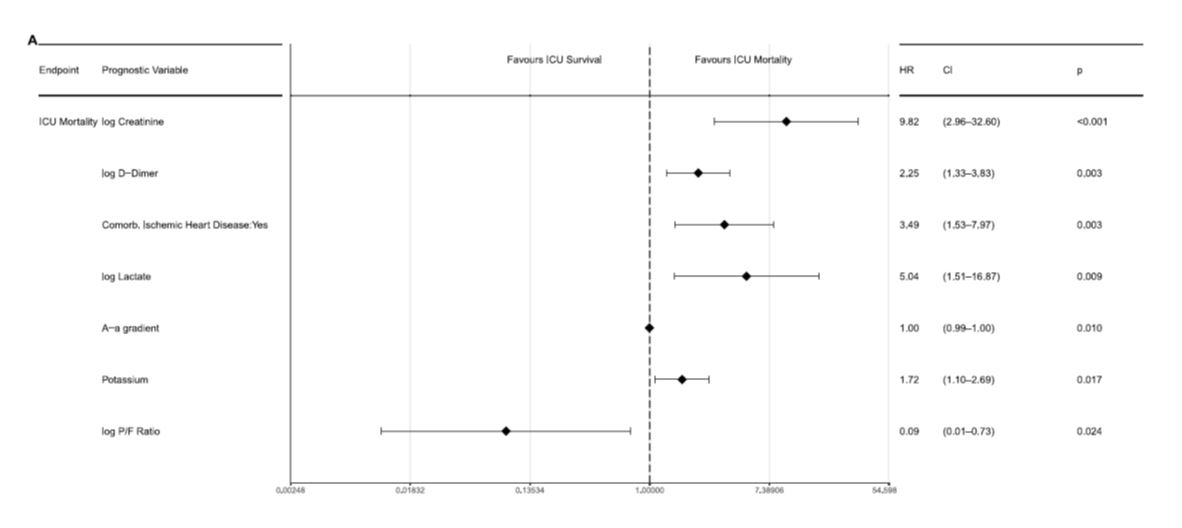
- data from patients admitted to the ICU in Switzerland (Wendel-Garcia) show that very few factors are independently associated with the risk of dying:
Uncertainty: reported death rates are highly variable, depending on the country, the type of patients included (general population, nursing home residents, ICU patients). Therefore, mortality data must be interpreted with caution. The total incidence and prevalence of infected patients in the population is unknown, mortality data have often been published early on the course of the pandemic (Baud), and death certificate do not always differentiate COVID-19 -related or non COVID-19 -related death. Definite and reproducible data on mortality will probably be available in the aftermath of the pandemic. In the meantime, age, male sex and co-morbid conditions are clearly associated with an increased risk of dying. As already mentioned, therapies with proven efficacy could modify the mortality and associated risks
Recommendations from the Task Force
There is a clear and probably independent association of age, male sex, and obesity for hospitalization, ICU admission, and mortality
Hospitalization Risk: Although age, male gender, obesity, comorbid state, chronic lung, heart or kidney disease, and diabetes have been associated with a higher risk of hospitalization, there are no validated prediction models that may help determine the proportion of patients needing hospital admission, or helping identifying the individual at risk.
ICU Admission Risk: Risk factors for hospitalization are similarly associated with a high risk of ICU admission, with the addition of dyspnea and ARDS (clinical or radiological) presentation at admission. However, published prediction models have not been validated in the Swiss population, so that they should be used very cautiously to identify the patient at risk for ICU admission.
Mortality risk: Age, male sex, obesity and chronic cardiovascular and lung disease, and ARDS presentation, have been associated with an unfavorable outcome. The 4C score is a simple prediction tool proposed by the WHO, but that has not been specifically validated in the Swiss population.
Open points for further discussion: Anti-viral and/or immunomodulating drugs use (mainly dexamethasone and remdesivir) may impact significantly the risk of ICU admission and death of COVID-19 patients in the months to come, but the amplitude of change is difficult to evaluate at this point.
Alqahtani JS, Oyelade T, Aldhahir AM, Alghamdi SM, Almehmadi M, Alqahtani AS, et al. (2020) Prevalence, Severity and Mortality associated with COPD and Smoking in patients with COVID-19: A Rapid Systematic Review and Meta-Analysis. PLoS ONE 15(5): e0233147. https://doi.org/10.1371/journal.pone.0233147
Bartoletti M, Giannella M, Scudeller L, Tedeschi S, Rinaldi M, Bussini L, Fornaro G, Pascale R, Pancaldi L, Pasquini Z, Trapani F, Badia L, Campoli C, Tadolini M, Attard L, Puoti M, Merli M, Mussini C, Menozzi M, Meschiari M, Codeluppi M, Barchiesi F, Cristini F, Saracino A, Licci A, Rapuano S, Tonetti T, Gaibani P, Ranieri VM, Viale P; PREDICO study group. Development and validation of a prediction model for severe respiratory failure in hospitalized patients with SARS-CoV-2 infection: a multicentre cohort study (PREDI-CO study). Clin Microbiol Infect. 2020 Aug 8:S1198-743X(20)30479-1. doi: 10.1016/j.cmi.2020.08.003. Epub ahead of print. PMID: 32781244; PMCID: PMC7414420.
Baud D, Qi X, Nielsen-Saines K, Musso D, Pomar L, Favre G. Real estimates of mortality following COVID-19 infection [published online ahead of print, 2020 Mar 12]. Lancet Infect Dis. 2020;S1473-3099(20)30195-X. doi:10.1016/S1473-3099(20)30195-X
CDC 2020. https://www.cdc.gov/coronavirus/2019-ncov/index.html. Accessed 24.4.2020
CEBM. https://www.cebm.net/COVID-19 /global-COVID-19 -case-fatality-rates/
Chen T, Wu D, Chen H, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study [published correction appears in BMJ. 2020 Mar 31;368:m1295]. BMJ. 2020;368:m1091. Published 2020 Mar 26. doi:10.1136/bmj.m1091
Docherty AB, Harrison EM, Green CA, et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ. 2020;369:m1985. Published 2020 May 22. doi:10.1136/bmj.m1985
Grasselli G, Zangrillo A, Zanella A, et al. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy [published online ahead of print, 2020 Apr 6]. JAMA. 2020;e205394. doi:10.1001/jama.2020.5394
Grasselli G, Greco M, Zanella A, et al. Risk Factors Associated With Mortality Among Patients With COVID-19 in Intensive Care Units in Lombardy, Italy. JAMA Intern Med. Published online July 15, 2020. doi:10.1001/jamainternmed.2020.3539
Grant MC, Geoghegan L, Arbyn M, et al. The prevalence of symptoms in 24,410 adults infected by the novel coronavirus (SARS-CoV-2; COVID-19): A systematic review and meta-analysis of 148 studies from 9 countries. PLoS One. 2020;15(6):e0234765. Published 2020 Jun 23. doi:10.1371/journal.pone.0234765
Gong J, Ou J, Qiu X, et al. A Tool to Early Predict Severe Corona Virus Disease 2019 (COVID-19 ) : A Multicenter Study using the Risk Nomogram in Wuhan and Guangdong, China [published online ahead of print, 2020 Apr 16]. Clin Infect Dis. 2020;ciaa443. doi:10.1093/cid/ciaa443
Guan WJ, Liang WH, Zhao Y, et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: A Nationwide Analysis [published online ahead of print, 2020 Mar 26]. Eur Respir J. 2020;2000547. doi:10.1183/13993003.00547-2020
Guan WJ, Ni ZY, Hu Y, et al. Clinical Characteristics of Coronavirus Disease 2019 in China [published online ahead of print, 2020 Feb 28]. N Engl J Med. 2020;NEJMoa2002032. doi:10.1056/NEJMoa2002032
Gupta S, Hayek SS, Wang W, et al. Factors Associated With Death in Critically Ill Patients With Coronavirus Disease 2019 in the US [published online ahead of print, 2020 Jul 15]. JAMA Intern Med. 2020;e203596. doi:10.1001/jamainternmed.2020.3596
Ioannidis JPA. Infection fatality rate of COVID-19 inferred from seroprevalence data. Bulletin of the World Health Organization; Article ID: BLT.20.265892
Jain V, Yuan JM. Predictive symptoms and comorbidities for severe COVID-19 and intensive care unit admission: a systematic review and meta-analysis. Int J Public Health. 2020 Jun;65(5):533-546. doi: 10.1007/s00038-020-01390-7. Epub 2020 May 25. PMID: 32451563; PMCID: PMC7246302.
Jehi, L., Ji, X., Milinovich, A., Erzurum, S., Merlino, A., Gordon, S., Young, J. B., & Kattan, M. W. (2020). Development and validation of a model for individualized prediction of hospitalization risk in 4,536 patients with COVID-19. PloS one, 15(8), e0237419.
Knight SR, Ho A, Pius R, Buchan I, Carson G, Drake TM, Dunning J, Fairfield CJ, Gamble C, Green CA, Gupta R, Halpin S, Hardwick HE, Holden KA, Horby PW, Jackson C, Mclean KA, Merson L, Nguyen-Van-Tam JS, Norman L, Noursadeghi M, Olliaro PL, Pritchard MG, Russell CD, Shaw CA, Sheikh A, Solomon T, Sudlow C, Swann OV, Turtle LC, Openshaw PJ, Baillie JK, Semple MG, Docherty AB, Harrison EM; ISARIC4C investigators. Risk stratification of patients admitted to hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: development and validation of the 4C Mortality Score. BMJ. 2020 Sep 9;370:m3339. doi: 10.1136/bmj.m3339. PMID: 32907855.
Lewnard JA, Liu VX, Jackson ML, et al. Incidence, clinical outcomes, and transmission dynamics of severe coronavirus disease 2019 in California and Washington: prospective cohort study. BMJ. 2020;369:m1923. Published 2020 May 22. doi:10.1136/bmj.m1923
Liang, W., Liang, H., Ou, L., Chen, B., Chen, A., Li, C., Li, Y., Guan, W., Sang, L., Lu, J., Xu, Y., Chen, G., Guo, H., Guo, J., Chen, Z., Zhao, Y., Li, S., Zhang, N., Zhong, N., He, J., 2020. Development and Validation of a Clinical Risk Score to Predict the Occurrence of Critical Illness in Hospitalized Patients With COVID-19. JAMA Internal Medicine.. doi:10.1001/jamainternmed.2020.2033
Liu W, Tao ZW, Lei W, et al. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease [published online ahead of print, 2020 Feb 28]. Chin Med J (Engl). 2020;10.1097/CM9.0000000000000775. doi:10.1097/CM9.0000000000000775
Mackey K, King VJ, Gurley S, et al. Risks and Impact of Angiotensin-Converting Enzyme Inhibitors or Angiotensin-Receptor Blockers on SARS-CoV-2 Infection in Adults [published online ahead of print, 2020 May 15]. Ann Intern Med. 2020;10.7326/M20-1515. doi:10.7326/M20-1515
Mancia G, Rea F, Ludergnani M, Apolone G, Corrao G. Renin-Angiotensin-Aldosterone System Blockers and the Risk of Covid-19 [published online ahead of print, 2020 May 1]. N Engl J Med. 2020;10.1056/NEJMoa2006923. doi:10.1056/NEJMoa2006923
MMWR. Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID-19 ) — United States, February 12–March 16, 2020. MMWR Morb Mortal Wkly Rep 2020;69:343-346. DOI: http://dx.doi.org/10.15585/mmwr.mm6912e2external icon.
Petrilli CM, Jones SA, Yang J, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020;369:m1966. Published 2020 May 22. doi:10.1136/bmj.m1966
Popkin BM, Du S, Green WD, Beck MA, Algaith T, Herbst CH, Alsukait RF, Alluhidan M, Alazemi N, Shekar M. Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships. Obes Rev. 2020 Nov;21(11):e13128. doi: 10.1111/obr.13128. Epub 2020 Aug 26. PMID: 32845580; PMCID: PMC7461480.
Qian Z, Alaa AM, van der Schaar M, Ercole A. Between-centre differences for COVID-19 ICU mortality from early data in England [published online ahead of print, 2020 Jun 22]. Intensive Care Med. 2020;1-2. doi:10.1007/s00134-020-06150-y
Reynolds HR, Adhikari S, Pulgarin C, et al. Renin-Angiotensin-Aldosterone System Inhibitors and Risk of Covid-19 [published online ahead of print, 2020 May 1]. N Engl J Med. 2020;10.1056/NEJMoa2008975. doi:10.1056/NEJMoa2008975
Richardson S, Hirsch JS, Narasimhan M, et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area [published online ahead of print, 2020 Apr 22]. JAMA. 2020;10.1001/jama.2020.6775. doi:10.1001/jama.2020.6775
Roncon L, Zuin M, Rigatelli G, Zuliani G. Diabetic patients with COVID-19 infection are at higher risk of ICU admission and poor short-term outcome [published online ahead of print, 2020 Apr 9]. J Clin Virol. 2020;127:104354. doi:10.1016/j.jcv.2020.104354
Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China [published online ahead of print, 2020 Mar 3] [published correction appears in Intensive Care Med. 2020 Apr 6;:]. Intensive Care Med. 2020;1–3. doi:10.1007/s00134-020-05991-x
Salive ME. Multimorbidity in Older Adults. Epidemiologic Reviews, Volume 35, Issue 1, 2013, Pages 75–83
Salje H, Tran Kiem C, Lefrancq N, et al. Estimating the burden of SARS-CoV-2 in France [published online ahead of print, 2020 May 13]. Science. 2020;eabc3517. doi:10.1126/science.abc3517
Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endotheliitis in COVID-19 [published online ahead of print, 2020 Apr 20]. Lancet. 2020;S0140-6736(20)30937-5. doi:10.1016/S0140-6736(20)30937-5
Verity R, Okell LC, Dorigatti I, et al. Estimates of the severity of coronavirus disease 2019: a model-based analysis [published correction appears in Lancet Infect Dis. 2020 Apr 15;:] [published correction appears in Lancet Infect Dis. 2020 May 4;:]. Lancet Infect Dis. 2020;20(6):669-677. doi:10.1016/S1473-3099(20)30243-7
Williamson EJ, Walker AJ, Bhaskaran K, et al. OpenSAFELY: factors associated with COVID-19 death in 17 million patients [published online ahead of print, 2020 Jul 8]. Nature. 2020;10.1038/s41586-020-2521-4. doi:10.1038/s41586-020-2521-4
Wendel-Garcia PD, Fumeaux T, Guerci P, Heuberger DM, Montomoli J, Roche-Campo F, Schuepach RA, Hilty MP. Prognostic factors associated with mortality risk and disease progression in 639 critically ill patients with COVID-19 in Europe: Initial report of the international RISC-19-ICU prospective observational cohort. E Clin Med. 2020 (published online July 6th 2020). DOI:https://doi.org/10.1016/j.eclinm.2020.100449
Wynants L, Van Calster B, Bonten MMJ, et al. Prediction models for diagnosis and prognosis of COVID-19 infection: systematic review and critical appraisal. BMJ. 2020;369:m1328. Published 2020 Apr 7. doi:10.1136/bmj.m1328
Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study [published correction appears in Lancet. 2020 Mar 28;395(10229):1038] [published correction appears in Lancet. 2020 Mar 28;395(10229):1038]. Lancet. 2020;395(10229):1054–1062. doi:10.1016/S0140-6736(20)30566-3
Zhang P, Zhu L, Cai Jingjing et al. Association of Inpatient Use of Angiotensin Converting Enzyme Inhibitors and Angiotensin II Receptor Blockers with Mortality Among Patients With Hypertension Hospitalized With COVID-19 .Circ Res. 2020 Apr 17. doi: 10.1161/CIRCRESAHA.120.317134.
Zhang JJY, Lee KS, Ang LW, Leo YS, Young BE. Risk Factors of Severe Disease and Efficacy of Treatment in Patients Infected with COVID-19: A Systematic Review, Meta-Analysis and Meta-Regression Analysis [published online ahead of print, 2020 May 14]. Clin Infect Dis. 2020;ciaa576. doi:10.1093/cid/ciaa576
Date of request: 19/4/2020
Date of update: 16/10/2020
In response to request from: NCS-TF Advisory Board
Comment on planned updates: This is a short systematic review by the group, based on the work of N. Müller (USZ) and T. Fumeaux (SGI). The document was updated on 16.10.2020, based on new published evidence.
Expert groups and individuals involved: Clinical Group
Contact persons: Nicolas Müller (Nicolas.Mueller@usz.ch) – Thierry Fumeaux (thierry.fumeaux@ghol.ch) – Manuel Battegay (Manuel.Battegay@usb.ch), Clinical Expert Group